Managing an autoimmune disease isn’t just about taking medication. It’s about staying one step ahead-catching flares before they hit, knowing if your treatment is working, and avoiding long-term damage to your organs. Many people think that if they feel fine, everything’s under control. But that’s not how autoimmune diseases work. Silent inflammation can be raging inside your body while you’re sleeping, eating, or walking the dog. That’s why structured monitoring-using lab tests, imaging, and regular check-ins-isn’t optional. It’s the difference between managing your condition and being managed by it.
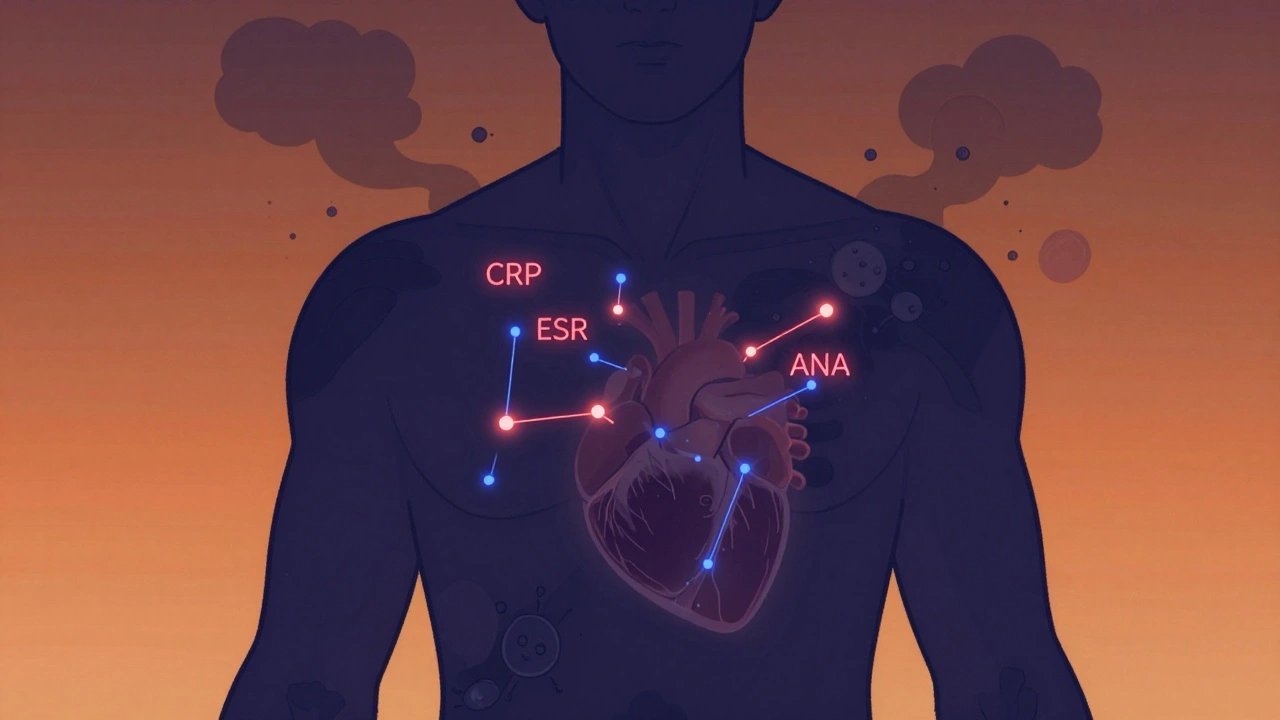
Lab Markers: What Your Blood Is Telling You
Your blood is a map of what’s happening inside. The most common tests used to track autoimmune diseases are CRP, ESR, and autoantibodies like ANA. CRP (C-reactive protein) rises quickly when inflammation flares up. A level above 3.0 mg/L is a red flag. ESR (erythrocyte sedimentation rate) moves slower but shows chronic inflammation. For women, anything over 20 mm/hr; for men, over 15 mm/hr, means something’s off. These aren’t diagnostic tests-they don’t tell you which disease you have-but they tell you if your body is in fight mode right now.
ANA (antinuclear antibody) is the gateway test. If you’ve been told you might have lupus, rheumatoid arthritis, or Sjögren’s, this is usually the first blood test ordered. It’s positive in 95% of lupus cases. But here’s the catch: 20% of healthy people also test positive. That’s why a positive ANA isn’t a diagnosis-it’s a signal to dig deeper. Reflex testing follows: if ANA is positive, labs check for specific antibodies like anti-dsDNA (strongly linked to lupus kidney involvement), SS-A and SS-B (Sjögren’s markers), Scl-70 (scleroderma), and Jo-1 (polymyositis). Anti-dsDNA is especially useful for tracking lupus activity. When it spikes, it often means your kidneys are under attack.
Don’t waste time retesting ANA every few months. It stays positive even during remission. Instead, watch complement levels-C3 and C4. When these drop, it’s a clearer sign that lupus is active. A 2023 study from UNC’s rheumatology department showed that patients who tracked complement levels had 41% fewer flare-ups than those who only checked ANA.
Imaging: Seeing What Blood Can’t Show
Lab tests tell you inflammation is there. Imaging tells you where and how badly. MRI is the gold standard for spotting early joint and tissue damage. It can detect swelling in tendons or synovium before you even feel pain. Newer contrast agents are safer than old gadolinium-based ones, which carried risks of kidney damage and brain deposits. Today’s nanotech agents are more targeted and break down faster.
Ultrasound is becoming a frontline tool, especially for rheumatoid arthritis. With acoustically active microbubbles, it measures blood flow in inflamed joints with 85% accuracy. It’s quick, cheap, and doesn’t use radiation. You can have it done in the rheumatologist’s office while you wait.
PET scans are the future. By tagging immune cells with radioactive tracers, doctors can now see where T-cells are congregating-like a heat map of your immune system’s misfires. A 2023 study used total-body PET to track inflammation in lupus patients and found activity in organs no one knew were involved. SPECT scans work similarly, using peptides that bind to inflammation markers to create 3D images of problem areas.
CT scans aren’t used for early detection-they’re too blunt. But when there’s suspected lung or organ damage from long-term disease, CT gives you the full picture. It’s not about radiation fear; it’s about knowing when damage has already happened.

Visits: The Human Element
No machine can replace your doctor’s eyes, ears, and hands. A patient might say they feel fine, but their hands are swollen. Or their gait has changed. Or they’re struggling to get out of a chair. These are clues lab results miss. The American College of Rheumatology says every patient with an autoimmune disease needs at least two full assessments a year: a physical exam, lab work, and a discussion about how they’re really doing.
When you’re newly diagnosed or your treatment just changed, you’ll likely see your doctor every 4 to 6 weeks. Once things stabilize, visits shift to every 3 to 4 months. But here’s the truth: many patients don’t get this. A 2023 Kaiser Family Foundation report found only 48% of Medicaid patients received recommended monitoring, compared to 83% of those with private insurance. That gap isn’t just unfair-it’s dangerous.
Doctors now use scoring systems to track progress. DAS28 for rheumatoid arthritis, SLEDAI for lupus. These scores combine joint counts, lab values, and patient reports into one number. If your score doesn’t improve over three visits, your treatment needs a rethink. It’s not about feeling better-it’s about hitting targets. That’s what EULAR’s treat-to-target guidelines are all about.
What’s Changing: Wearables, AI, and the Future
The old model-come in every few months, get a blood draw, wait a week for results-is fading. New tools are changing the game. Wearables are now being tested to measure inflammatory markers through interstitial fluid. Early studies show they match traditional CRP readings 89% of the time. Imagine wearing a patch that alerts you to a flare before your joints ache.
AI is stepping in too. In 2024, a study in Autoimmunity Reviews showed an algorithm could predict flares 14 days in advance by analyzing your past lab results, medication history, sleep patterns, and symptom logs. That’s not sci-fi-it’s FDA-approved. The platform AutoimmuneTrack, cleared in mid-2023, cut emergency visits by 29% in a trial of over 2,300 patients.
But tech isn’t magic. It’s a tool. Dr. Betty Hahn from UNC says, “Relying solely on lab values misses critical clinical context present in 63% of autoimmune flares.” You need all three: labs, imaging, and human judgment. That’s the 30-30-40 rule experts now follow: 30% weight on lab markers, 30% on imaging, 40% on clinical assessment.
Barriers and Real-World Challenges
Not everyone has equal access. ANA test results vary by 22% between labs because of differences in equipment and protocols. Insurance often denies MRIs or PET scans unless you’ve failed three other treatments. Out-of-pocket costs for a single PET scan can hit $3,000. That’s why many patients skip them-even when their doctor recommends it.
High-risk patients-those with kidney, lung, or nervous system involvement-need quarterly monitoring. Stable patients with mild disease might only need checks every 6 to 12 months. But too many doctors still use a one-size-fits-all approach. Personalization is the new standard.
The global market for autoimmune monitoring is now $12.7 billion, growing fast. But money doesn’t always reach the people who need it most. If you’re struggling to afford tests, ask your doctor about patient assistance programs. Many labs offer sliding scales. Nonprofits like the Autoimmune Association can help navigate insurance hurdles.
Monitoring isn’t about fear. It’s about control. It’s about knowing you’re not just reacting to flares-you’re preventing them. Every blood draw, every scan, every visit is a piece of the puzzle. Put them together, and you see the whole picture. And that’s how you take back your life.
How often should I get lab tests for my autoimmune disease?
It depends on your disease and how stable it is. When you’re newly diagnosed or adjusting treatment, expect blood tests every 4 to 6 weeks. Once your condition is under control, most doctors recommend tests every 3 to 4 months. For stable, low-risk patients, twice a year may be enough. Always follow your rheumatologist’s plan-don’t skip tests just because you feel fine.
Is a positive ANA test enough to diagnose an autoimmune disease?
No. A positive ANA is a screening tool, not a diagnosis. Up to 20% of healthy people have a positive ANA without any autoimmune disease. What matters is the pattern and whether other autoantibodies are present. If ANA is positive, your doctor will order reflex tests like anti-dsDNA, SS-A, or Scl-70 to narrow down the condition. Diagnosis always combines lab results, symptoms, and physical findings.
Why do I need imaging if my blood tests are normal?
Blood tests show inflammation, but not where it’s happening or how much damage has been done. You can have normal CRP and ESR but still have early joint erosion, lung scarring, or nerve inflammation-things only MRI, ultrasound, or PET can detect. Imaging finds silent damage before it becomes permanent. That’s why even with normal labs, your doctor may still recommend scans if you have symptoms.
Can wearable devices replace lab tests for autoimmune monitoring?
Not yet. Wearables that track inflammatory markers through skin fluid are promising-they’ve matched CRP levels 89% of the time in early studies. But they can’t replace full lab panels that check for specific autoantibodies, complement levels, or organ function. Think of wearables as early warning systems, not diagnostic tools. They’re best used alongside regular blood tests and doctor visits.
What should I do if my insurance won’t cover recommended scans or tests?
Ask your doctor to write a letter of medical necessity explaining why the test is critical for your care. Many labs offer payment plans or discounts for uninsured or underinsured patients. Nonprofits like the Autoimmune Association and Patient Advocate Foundation can help you appeal denials or find free testing programs. Don’t give up-your health is worth fighting for.
Do I need to get an MRI every year if I have lupus?
No, not unless your doctor recommends it. Routine yearly MRIs aren’t standard unless you have symptoms like unexplained headaches, vision changes, or joint pain that don’t match your lab results. MRIs are used when there’s suspicion of organ involvement-like brain, kidney, or lung damage. Your doctor will order imaging based on your individual risk, not on a fixed schedule.
Webster Bull
Feeling fine doesn't mean you're safe. I learned that the hard way. My CRP was normal for months, but my knees were turning to dust. Turns out, inflammation was hiding in the synovium. Ultrasound caught it before the damage was permanent. Don't wait for pain to scream at you.
Bruno Janssen
I hate how doctors treat us like numbers. I get the labs, I get the scans, but no one ever asks if I slept. Or if I cried last night. Or if I'm scared to even leave the house. They think tracking markers fixes everything. It doesn't.
Scott Butler
Why are we letting tech companies dictate healthcare? Wearables? AI? Next they'll be selling us 'autoimmune patches' on Amazon. This is why America's medical system is broken-overcomplicating simple things with gadgets. Just give me a good doctor and a blood test.
Emma Sbarge
The 30-30-40 rule is spot on. I’ve seen too many patients get discharged because their CRP was low, then end up in the ER three weeks later with kidney failure. Labs are a piece. Imaging is another. But the human assessment? That’s the lifeline. Don’t let insurance cut that corner.
Donna Hammond
For anyone reading this and feeling overwhelmed: you’re not alone. I had lupus for 12 years before I found a rheumatologist who actually listened. I track my complement levels monthly, log my sleep and stress in a notebook, and use the DAS28 score to talk to my doctor. It’s not magic, but it’s mine. And it’s kept me out of the hospital for 5 years straight. You can do this.
Richard Ayres
It’s fascinating how the field is evolving. The shift from reactive to predictive care is monumental. That AI model predicting flares 14 days in advance? That’s not just innovation-it’s a paradigm shift. But as the post says, it’s a tool, not a replacement. The human element remains irreplaceable, especially when emotions, fatigue, and subtle behavioral shifts are involved.
Sheldon Bird
Just had my first PET scan last month. Saw a hot spot in my lungs I didn’t even know was there. Felt weird seeing my own immune system on fire like a heatmap. But honestly? It gave me peace. Now I know what I’m fighting. And I’m not just guessing anymore. 🙌
Michael Gardner
Wait-so we’re supposed to believe a $3,000 PET scan is necessary for everyone? My cousin with RA got a $12,000 bill for one and still got denied coverage. This isn’t medicine, it’s a luxury service for the rich. The real issue isn’t monitoring-it’s access.
Willie Onst
Hey, I’m from the Philippines but living in Texas now. Back home, we don’t have half this tech. But we have family who notice when you’re off-how you walk, how you eat, how you laugh less. Maybe the real monitoring system was never the machine. Maybe it was always the people who love you enough to say, 'You don’t look right.' Just saying.






Write a comment