
When a patient walks into the ER with shortness of breath, the clock starts ticking. Is it heart failure? COPD? A pulmonary embolism? Ordering the wrong test can mean delays, unnecessary scans, or even missed diagnoses. That’s where NT-proBNP comes in - a simple blood test that can cut through the noise and give you a clear answer in under an hour.
Why NT-proBNP Is the Go-To Test for Suspected Heart Failure
NT-proBNP stands for N-terminal pro-B-type Natriuretic Peptide. It’s a protein released by the heart when its walls are stretched from too much pressure - a telltale sign of heart failure. Unlike symptoms like swelling or fatigue, which can be caused by many things, NT-proBNP gives you hard, measurable data. It’s not a guess. It’s a number.
The test has become the gold standard because it’s incredibly good at ruling heart failure out. If the level is below 300 pg/mL, there’s a 98% chance the patient doesn’t have acute heart failure. That’s not a small edge - it’s a game-changer. In emergency departments across Australia, the U.S., and Europe, this single number has cut unnecessary hospital admissions by up to 19%. One study found that after implementing NT-proBNP testing, hospitals reduced the number of echocardiograms ordered by nearly a quarter. That means less cost, less waiting, and less stress for patients.
When to Order It - The Clinical Scenarios That Demand NT-proBNP
You don’t order this test for every patient with a cough. But there are clear, well-supported situations where it’s not just helpful - it’s essential.
- Patients presenting with acute dyspnea - especially those over 65. If someone comes in gasping for air and you’re not sure if it’s heart failure or something else, NT-proBNP is your first step. The European Society of Cardiology gives it a Class I recommendation - meaning it’s a must-do.
- Patients with known heart disease who develop new symptoms - like sudden weight gain, reduced exercise tolerance, or nighttime breathing trouble. A rising NT-proBNP level can tell you the disease is worsening before you even see fluid on a chest X-ray.
- Patients with atrial fibrillation and unexplained shortness of breath - this combo is tricky. AFib can elevate NT-proBNP on its own, but if the level is sky-high (say, over 1,500 pg/mL), it’s a red flag for heart failure on top of the arrhythmia.
- Post-heart attack patients with signs of stress - new guidelines now recommend NT-proBNP testing within 24 hours after an acute coronary syndrome to identify those at highest risk for future heart failure events.
Here’s what you don’t order it for: routine checkups, asymptomatic patients, or as a screening tool in healthy people. Medicare data shows 18% of tests are ordered in people with no symptoms - and that’s waste. Starting January 2025, CMS will require prior authorization for these low-yield cases. Don’t be the doctor who orders it just because it’s easy.
How to Interpret the Numbers - Age, Kidneys, and Other Confounders
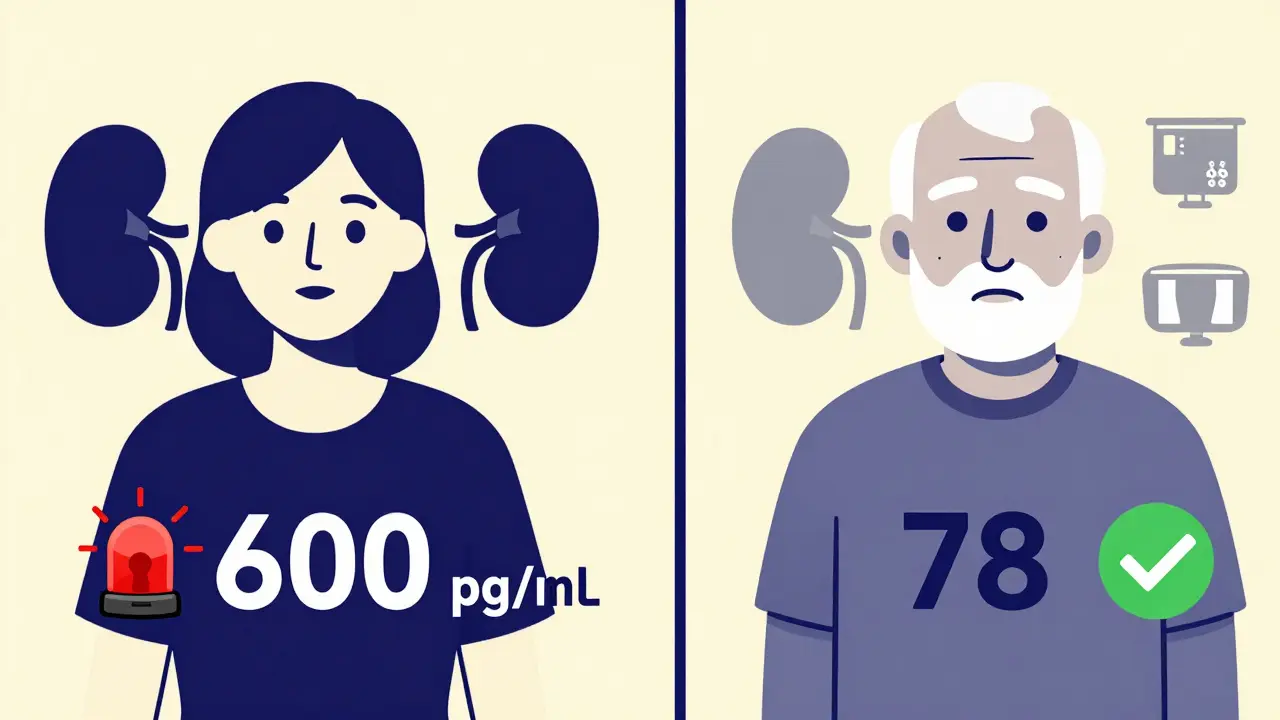
The number itself isn’t enough. You have to read it in context. NT-proBNP levels rise naturally with age. A 70-year-old with 600 pg/mL might be perfectly normal. A 35-year-old with the same level? That’s a red flag.
Here’s the practical guide:
| Group | Rule-Out Threshold (pg/mL) | Diagnostic Threshold (pg/mL) |
|---|---|---|
| Under 50 years | 300 | 450 |
| 50-75 years | 300 | 900 |
| Over 75 years | 300 | 1,800 |
| CKD Stage 3-5 | 1,200 | 2,500 |
| Obesity (BMI >30) | 300 | Lower than expected - interpret cautiously |
Renal failure is the biggest trap. Kidneys clear NT-proBNP. If they’re not working, the level climbs - even without heart failure. In patients with stage 3-5 chronic kidney disease, the rule-out threshold jumps from 300 to 1,200 pg/mL. Miss that adjustment, and you’ll overdiagnose heart failure in half the patients with advanced kidney disease.
Obesity is another curveball. Fat tissue suppresses NT-proBNP release. A person with a BMI of 40 might have levels 25-30% lower than expected for their heart condition. So if their number is borderline, don’t dismiss heart failure just because it’s "not high enough."
What NT-proBNP Can’t Do - And What to Do Instead
This test is powerful, but it’s not magic. It doesn’t tell you why the heart is failing. It doesn’t show you if there’s a blocked artery or a leaky valve. It doesn’t replace echocardiography - it tells you when you need it.
Here’s what to do when the number is confusing:
- NT-proBNP is 850 pg/mL in a 78-year-old with AFib and CKD - this is the classic gray zone. Don’t panic. Look at the trend. Was it 400 last year? Then it’s likely worsening heart failure. Was it always around 800? Then it’s probably baseline. Repeat the test in 48 hours if you’re unsure.
- NT-proBNP is normal, but the patient still looks like heart failure - think outside the box. Is it pericardial effusion? Constrictive pericarditis? Restrictive cardiomyopathy? These conditions don’t always raise NT-proBNP. You’ll need imaging.
- NT-proBNP is sky-high, but the patient feels fine - this happens. It could mean silent heart failure, or it could be an artifact. Check for recent infection, uncontrolled hypertension, or pulmonary embolism. A high level in an asymptomatic person still needs investigation.
Remember: NT-proBNP is a tool. It’s not a diagnosis. You need the full picture - history, physical exam, ECG, and sometimes imaging.
What’s Changing in 2025 - And What You Need to Know
The field is moving fast. In 2023, the FDA cleared the first point-of-care NT-proBNP device - the Roche Cobas h 232 - that gives results in 12 minutes. That’s a game-changer for rural clinics and ERs without on-site labs. You’ll be able to test, interpret, and act before the patient leaves the room.
The 2024 ACC/AHA/HFSA guidelines, due for release in September, will expand NT-proBNP use to risk-stratify patients after heart attacks. If their level drops by more than 30% in the first 72 hours, their risk of death or hospitalization drops by 35%. That’s not just diagnostic - it’s prognostic.
And then there’s the cost. Medicare reimburses $18.42 per test. But if you order it inappropriately - like for an asymptomatic 60-year-old with no symptoms - you’ll get flagged. Starting January 2025, prior authorization will be required for tests without clear clinical indication. That means documentation matters. If you don’t write "suspected acute heart failure" or "new dyspnea in patient with known CAD," you’ll get denied.

Real-World Impact - What Clinicians Are Saying
A cardiologist in Melbourne shared this case: An 82-year-old woman with COPD came in with worsening breathlessness. Her oxygen was low. Her lungs were wheezy. She was on three inhalers. Everyone assumed it was a COPD flare. But the NT-proBNP came back at 120 pg/mL. That ruled out heart failure. She didn’t get a costly echo. She didn’t get diuretics that made her dizzy. She got a lung CT - which found a pulmonary embolism. She was treated and discharged in 48 hours.
Another clinician on a medical forum wrote: "I used to order echos for every older patient with shortness of breath. Now I order NT-proBNP first. It’s cut my echo workload by 60%. And I’ve stopped sending patients home with wrong diagnoses."
That’s the power of this test. It’s not flashy. It doesn’t make headlines. But it changes outcomes - every day, in real time.
Is NT-proBNP the same as BNP?
No. BNP (B-type Natriuretic Peptide) is the active hormone, while NT-proBNP is its inactive fragment. NT-proBNP is more stable in blood, lasts longer in circulation (up to 2 hours vs. 20 minutes for BNP), and is less affected by sample handling. That’s why most labs now prefer NT-proBNP. It’s more reliable, especially if there’s a delay in testing.
Can NT-proBNP be used to monitor heart failure treatment?
Yes - but not as a daily tracker. It’s most useful for tracking trends over weeks or months. A falling NT-proBNP level after starting a new heart failure medication (like an SGLT2 inhibitor or ARNI) suggests the treatment is working. A rising level may mean the disease is progressing or the patient isn’t adhering to therapy. It’s not meant for real-time adjustments - that’s what symptoms and physical exams are for.
Do I need to fast before an NT-proBNP test?
No. Unlike cholesterol or glucose, NT-proBNP levels aren’t affected by food, drink, or time of day. You can test at any time, even after a meal. The only requirement is a standard serum sample - no special tubes needed.
What if the NT-proBNP is normal but the patient still has symptoms?
A normal NT-proBNP (below 300 pg/mL) effectively rules out acute heart failure. But if symptoms persist, look elsewhere. Could it be lung disease, anemia, thyroid dysfunction, or anxiety? Don’t force a heart failure diagnosis because the patient "feels like they have it." Use the test as a gatekeeper - if it’s negative, move on to other causes.
Are there any new alternatives to NT-proBNP?
Multi-marker panels (like ST2, GDF-15, galectin-3) are being studied, but none have replaced NT-proBNP. It’s still the strongest predictor of heart failure outcomes, with over 28 years of outcome data backing it. Emerging tests may add nuance, but NT-proBNP remains the foundation. Don’t wait for the next big thing - master this one first.
Final Takeaway - Order Smart, Interpret Smart
NT-proBNP testing isn’t optional anymore. It’s standard care. But like any tool, it’s only as good as the person using it. Order it when there’s real suspicion of heart failure. Know the cutoffs for age and kidney function. Don’t let a number override clinical judgment. And never use it as a fishing expedition.
When done right, this test saves time, money, and lives. It turns uncertainty into clarity. And in medicine, that’s worth more than any machine.





