
Picture this: it’s three in the morning and you’re doubled over with pain that started after a simple trip to the restroom. Your doctor’s diagnosis? A urinary tract infection. The most common script: Cipro. Also known as ciprofloxacin, this antibiotic has a reputation for clearing up stubborn infections fast. But is this go-to drug always the magic fix everyone thinks it is? Not exactly. The story of Cipro is laced with lifesaving success, real risks, misunderstandings, and a few mistakes worth learning from. With the right info, you can tell if Cipro deserves a spot in your medicine cabinet—or if you should look for other options.
How Does Cipro Work and What Does It Treat?
Ciprofloxacin belongs to a powerful family of antibiotics called fluoroquinolones. Its job? Stop certain types of bacteria right in their tracks. Think of it as a chemical wrench tossed straight into bacteria’s genetic machinery: it blocks the enzymes needed for those bugs to copy DNA. Without that, the harmful bacteria can’t multiply. What kinds of germs fall to Cipro? Mainly Gram-negative bacteria—like Escherichia coli (E. coli), Klebsiella, and Pseudomonas—often the main villains in urinary tract infections (UTIs), kidney infections, infectious diarrhea, complicated respiratory infections, and more. But Cipro isn’t just for basic bugs. It's been used for exposure to anthrax, bone and joint infections, and even some stubborn sinus and prostate infections.
Doctors have leaned on Cipro for decades because it works fast and tackles otherwise tough-to-treat infections. It’s available as pills, liquids, and even IV drips in hospitals. Hospitals sometimes use it after exposure to biological threats or in cases where traditional antibiotics have failed. The US Food and Drug Administration (FDA) first approved Cipro in 1987, and it made headlines in 2001 during the anthrax scare. If you checked your hospital’s pharmacy cabinet even today, there’s a good chance you’d spot it near the top shelf.
Despite its usefulness, Cipro has limits. It doesn't do anything for viruses. Got the flu, a cold, or COVID-19? Cipro won’t help. Don't expect it to work on run-of-the-mill strep throat: it doesn’t cover most Gram-positive bacteria well. Some countries and medical guidelines now recommend Cipro only for certain conditions, to slow rising antibiotic resistance. If you’ve taken Cipro and it didn’t work, there’s likely a reason—the bacteria might be resistant, or the infection wasn’t caused by the right type of bacteria in the first place. Doctors now test urine, blood, or sputum samples in the lab to check if a bug is sensitive to Cipro before prescribing it.
Though it’s powerful, Cipro isn’t a universal fix. The Centers for Disease Control and Prevention (CDC) reports around 30% of E. coli urinary infections now show resistance in some regions. Still, Cipro can be the right choice when prescribed with care and for the right infection. Knowing how it works and when it’s needed is half the battle when you’re dealing with tough bacterial invaders.
Cipro Side Effects: The Good, The Bad, and The Surprising
No medicine is all benefit, no risk—and Cipro is the poster child for weighing both. The mild stuff? About 1 in 10 people using Cipro might get loose stools, some nausea, an upset stomach, or even a weird taste in the mouth. Most of these, thankfully, go away once you stop the drug or finish your prescription. Occasionally you’ll see someone get dizzy, fatigued, or struggle with headaches. Some folks notice a rash, itch, or sunburn much faster than usual—Cipro does make you a tad more sensitive to sunlight, so sunscreen is not just for the beach anymore.
But Cipro’s darker side has gotten a lot more attention over the years. The FDA started slapping “black box” warnings on Cipro after serious side effects came to light. Tendon tearing—the stuff usually reserved for athletes—can actually happen to regular users of Cipro, especially people over 60, those using steroids, or folks with kidney issues. The most notorious case involves the Achilles tendon, but any tendon can be at risk. The pain can start days or weeks into treatment or, in rare cases, months after your last dose. If you ever feel a snap or sudden pain in a joint after starting Cipro, that’s your sign to get checked right away.
The nerves can take a hit, too. Some people develop tingling, burning, numbness, or weakness in hands or feet —a condition called peripheral neuropathy. Even more worrying, some of these nerve problems can be long-lasting or even permanent. The odds are low, but the risk is real.
Mood changes, insomnia, even hallucinations have shown up in younger people and older adults on Cipro. Suddenly having trouble thinking clearly, feeling anxious out of the blue, or having scary dreams? Doctors now know Cipro can cross the blood-brain barrier. For those with a history of mental health issues, pay extra attention to any brain fog or strange mood swings.
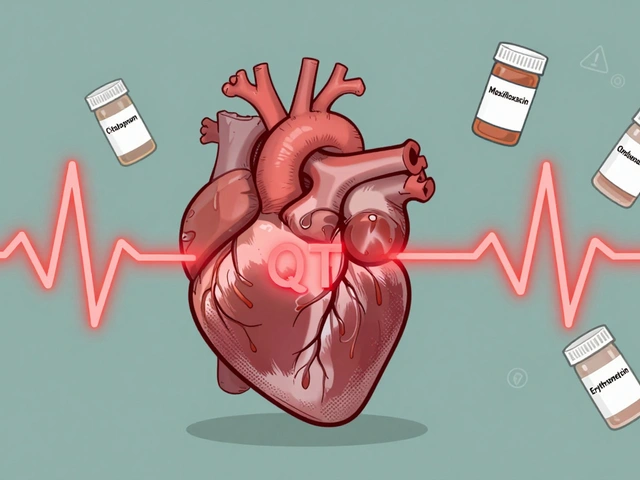
If you’ve ever had a history of heart problems, listen up. Cipro can lead to changes in how your heart beats, specifically prolonging the QT interval on an EKG. For most, this means nothing. But for those already on medications that affect the heart, or who have a family history of sudden cardiac death, ask for a heart check before starting Cipro. It could make a difference.
Here’s a look at Cipro side effect numbers, so you can see the difference between common and rare risks:
| Side Effect | Approximate Occurrence Rate |
|---|---|
| GI Upset (Nausea, Diarrhea) | Up to 10% |
| Rash/Photosensitivity | 2-3% |
| Headache | 1-2% |
| Tendon Rupture | 0.1% |
| Peripheral Neuropathy | 0.1-0.2% |
| Serious Mood/Brain Effects | Low, but can happen in any age |
Still, millions take Cipro without problems. The trick is having an honest talk with your doctor about your health history and reporting any strange symptoms—fast.

Smart Tips for Taking Cipro: What Actually Works
If your doctor calls in a Cipro prescription, start with some simple advice: read the information sheet, but don’t get overwhelmed. Most people take Cipro by mouth, twice a day, usually for 3 to 14 days depending on the infection. Always stick with what your doctor recommends: some infections, like anthrax or bone infections, might require longer courses or IV forms in hospitals.
- Stick to a schedule. Try to take Cipro at the same times every day. If you forget a dose and it's close to your next dose, skip the missed one—don’t double up.
- Take Cipro with a full glass of water. Drink plenty of fluids throughout the day, unless your doctor tells you to limit liquids.
- Avoid dairy or calcium supplements within 2 hours before and after your dose. Calcium can bind to Cipro in your stomach, making it much less effective. That goes for antacids, iron supplements, or multivitamins too.
- If you love the sun, use sunscreen and try to stay cool. Cipro can make your skin burn fast—what’s fine one day could turn nasty the next.
- If you work out or play sports, pay attention to your joints. Report pain, swelling, or odd stiffness to your doctor right away.
- Tell your doctor about all your meds—especially arrhythmia drugs, blood thinners, or insulin. Some drugs interact with Cipro and amp up side effects or blunt effectiveness.
Don’t stop your prescription early even if you feel better. Incomplete courses help create resistant bacteria—superbugs that are hard to kill and dangerous for everyone. If you’re throwing up or have severe diarrhea, call your doctor instead of just quitting. And always finish your prescription even if the bottle seems bottomless. Bacteria have a nasty habit of coming back if you give them a second chance.
Cipro isn’t your everyday, low-key antibiotic. If you have a history of tendon issues, muscle disorders, epilepsy/seizures, or serious heart disease, make sure your healthcare provider knows. Young kids and pregnant women usually get a different antibiotic since the risk of joint damage is higher in growing bodies. For older adults—especially those on steroids, diuretics, or with kidney disease—the risks get a bit higher. Best tip: make a personal medication list, carry it, and let your healthcare team know what’s on it every time you see them.
What about alcohol? On its own, moderate drinking is not clearly banned with Cipro, but if you mix booze with a body already fighting infection or taking other meds, expect dehydration or more side effects. Bit of common sense here—skip happy hour until you’re feeling better.
What’s Next? Resistance, Alternatives, and New Research on Ciprofloxacin
Doctors used to hand out Cipro for nearly everything from sinus infections to gut bugs. Now, the tide is turning. With so many bacteria developing resistance—and side effect warnings stacking up—most doctors are more cautious. The World Health Organization even lists fluoroquinolones as a ‘Watch Group’ antibiotic, meaning they need careful stewardship to prevent the rise of superbugs nobody can treat.
If your infection doesn’t call for Cipro, your doctor might opt for another drug like nitrofurantoin (for uncomplicated UTIs), amoxicillin-clavulanate, or a cephalosporin. Think of this as “rotation” to keep bacteria guessing and resistance lower. For serious hospital infections—like pseudomonal pneumonia or bone infections—Cipro or its cousin levofloxacin are sometimes still necessary. On the flip side, the FDA now recommends against using Cipro as a first-line treatment for simple sinus or bronchitis problems unless nothing else works.
Researchers in 2024 published a series of studies in JAMA, showing that Cipro’s risk for muscle and nerve problems may be higher than once thought—especially in people with autoimmune conditions or past tendon injuries. Another recent finding: some E. coli strains spreading in North America are now resistant to Cipro, making lab testing more important each year. Public health specialists urge patients to ask for cultures instead of jumping into antibiotics blind—the extra two or three days of waiting can mean less risk, fewer surprises, and the right medicine for the job.
Meanwhile, drug companies are working on newer fluoroquinolones that try to keep the power but dodge some of those bad side effects. No magic bullet has replaced Cipro yet. But your best defense? Staying informed, having real conversations with your doctor, and always finishing the right course—never sharing leftover antibiotics or using old prescriptions from last year’s drawer.
If you’ve had issues with Cipro in the past—or if a close family member had tendon rupture or nerve trouble—tell your next doctor before starting any new antibiotic. Honest, specific conversations can help keep you safer, help doctors track patterns, and maybe even push for better antibiotics down the line. With all this on the table, you’re better equipped to make smart choices the next time someone slips a Cipro script your way.
Christine Watson
This article is a great read for anyone prescribed Cipro. I appreciate how it breaks down the key points about what this antibiotic treats and shares important safety tips. It's reassuring to know the side effects to watch for, especially since antibiotics can sometimes cause unexpected reactions.
One thing I always ask my doctor is about interactions with other medications or supplements I’m taking, so it’s really helpful the article highlights that. Has anyone else felt unsure about when exactly to take their dose in relation to meals or other meds? This kind of info is crucial for avoiding problems.
Overall, this kind of detailed explanation helps patients become more informed and confident about taking their prescriptions responsibly, which is super important. Thanks for sharing!
Macy Weaver
I have always been curious about antibiotics like Cipro because sometimes the risks sound so scary! This article nicely outlines both uses and side effects without being too technical. I do wonder though, Cipro is often prescribed for everything from urinary tract infections to respiratory issues—are there specific infections where it’s absolutely preferred over others?
Also, it mentions essential tips for taking it safely. Could someone clarify how closely we need to follow timing? Like, if you miss a dose by a couple hours, is it a big deal? I guess these are the kind of questions I'd definitely want to ask my doctor to avoid pitfalls.
Really appreciate the focus on real risks and encouraging us to be proactive with our health care providers.
James McCracken
While this post offers a seemingly thorough overview of Cipro, I can’t help but question the underlying trust in pharmaceuticals at large. We’re so quick to accept these antibiotics without fully digesting the long-term consequences or the implications of overuse.
It would be interesting if the article addressed antibiotic resistance directly, given Cipro’s extensive application. Are we just feeding into a cycle where drugs lose efficacy because the bacteria evolve faster than our meds?
The mention of ‘real risks’ is there, but what about broader societal risks? It requires a more critical perspective than just listing side effects and doses. Anyone else feel the need for a more skeptical lens regarding these medications?
Evelyn XCII
Oh joy, another antibiotic overview that probably reads like a pamphlet your doctor hands you when you’re half-asleep. Cipro this, side effect that—yawn. Spoiler alert: if you’re allergic or reckless, you’ll know it.
Anyway, if you want the short version, here it is: don’t mess around with antibiotics. Follow orders, be mindful, and maybe, just maybe, it’ll do its job without turning you into a science experiment.
For those needing dramatic flair: yes, it can be dangerous if you ignore the warnings. But no one enjoys being the cautionary tale of antibiotic misuse. Stay safe, people, or you’ll be back here whining about tendonitis.
Nina Vera
OMG y’all, I had the craziest experience with Cipro last year! Seriously, this stuff is no joke. I was prescribed it for a stubborn infection, and within days, I felt like my joints were ON FIRE. Reading about tendon issues in this article gave me chills — I totally ignored the warnings and paid the price.
If you’re even THINKING about taking Cipro, please read ALL the warnings carefully. It can be a lifesaver but also a drama magnet. I was bedbound for weeks, and the side effects honestly made me question my life choices.
Anyway, thanks for sharing the facts! Hopefully more folks will take the risks seriously before they end up like me, limping and regretting it.
Daniel Buchanan
This write-up is pretty comprehensive, and I particularly appreciate that it encourages patients to ask questions. Doctors don’t always share everything unless you prompt them. For instance, I always ask if Cipro could affect my gut flora long-term, or if there’s a need to balance it with probiotics.
Side effects like nausea and dizziness are mentioned a lot, but what about rarer neurological side effects? I read somewhere that some patients have neuropathy symptoms long after stopping. Has anyone encountered that or read reliable research?
Also, the bit about drug interactions is crucial. Antibiotics often interact with common meds, which can catch people off guard.
Lena Williams
I can't help but think about how the article briefly mentions ‘safe use’ but doesn’t dive deep into what that entails beyond following your prescription. For instance, do lifestyle factors like hydration, diet, or even exercise impact the effectiveness or side effects of Cipro? I've heard caffeine can irritate the stomach more when taking antibiotics, is that well-founded or just a myth?
Also, I find the advice to always 'ask your doctor' is standard, but for many, that conversation can be intimidating or rushed. I wish there were more resources on how to communicate effectively about medication concerns.
This article is a good step toward patient education but leaves me wanting more nuanced guidance.
Sierra Bagstad
From a clinical perspective, this article manages to condense key pharmacological aspects of ciprofloxacin quite accurately. It highlights the drug’s breadth in combating various bacterial infections effectively.
Nonetheless, I would emphasize the importance of adherence to prescribed dosage schedules to prevent resistance development. It is equally crucial to monitor for adverse effects, especially tendinopathy and QT prolongation, which are well-documented.
Patients must be aware that ciprofloxacin is contraindicated in those with a history of hypersensitivity and must exercise caution when combined with other QT-prolonging agents. Overall, a sound summary, but we can never stress enough the significance of medical oversight.
Kemari Nielson
It’s refreshing to see a post that doesn’t just drop a list of side effects but encourages patients to actually understand what they’re taking. That said, I find a bit of balance is necessary—antibiotics like Cipro are powerful but shouldn’t be demonized either.
Following directions is imperative, and understanding when not to take it (like with some muscle or tendon issues) can save a lot of trouble. Has anyone here managed to use Cipro successfully without major side effects? Tips would be appreciated!
Steve Helsel
Thanks to everyone for the various takes! Just wanted to add one tiny thing: it’s vital to complete the entire antibiotic course, even if you start to feel better early on. Skipping doses or stopping prematurely can contribute heavily to resistance—which is something this post indirectly encourages by highlighting ‘safe use’.
I say this as someone who’s seen cases spiral due to impatience with meds. Also, if you experience side effects beyond mild ones, definitely check back with your healthcare provider. Early intervention is key and might prevent bigger issues down the line.
Steve Moody
Well, well, well, if it weren’t the quintessential rundown on Cipro, complete with the expected caveats about side effects and inquiries to pose to one’s doctor.
To add to the discourse with the subtlety of a sledgehammer: anyone dismissing the severity of risks such as tendon rupture or CNS effects is ignoring centuries of pharmacological data and medical history. Precision in dosage timing, awareness of contraindications, and monitoring for adverse reactions are not optional; they are prerequisites for safe therapy.
Moreover, a superficial overview, while informative, cannot replace the rigor of professional consultation. Hence, please, let us not reduce this crucial medication to a mere checkbox on your to-do list without proper respect.



Write a comment