
Most people assume that if a doctor prescribes a medication, it’s safe. But some drugs quietly scar your lungs-long before you feel any symptoms. Drug-induced pulmonary fibrosis (DIPF) isn’t rare. It’s not a glitch. It’s a known, documented, and often overlooked side effect of medicines millions take daily. And once the scarring sets in, it doesn’t heal.
What Happens When a Drug Turns Your Lungs to Scar Tissue
Your lungs aren’t just air sacs. They’re delicate networks of tissue that exchange oxygen and carbon dioxide. Pulmonary fibrosis means that tissue gets replaced by stiff, fibrous scar tissue. It’s like your lungs slowly turn to parchment. You don’t notice at first. Maybe you’re just out of breath climbing stairs. Or you’ve had a dry cough for months and assumed it was allergies. But when the scarring builds up, your lungs can’t expand. Oxygen can’t reach your blood. And no pill can undo it. This isn’t caused by smoking or pollution. It’s caused by drugs. And the worst part? It doesn’t happen to everyone. One person takes amiodarone for 18 months and stays fine. Another takes it for six months and ends up on oxygen. Why? We don’t fully know. Genetics, age, existing lung health-all play a role. But the trigger? The medicine.The Top 5 Medications That Can Scar Your Lungs
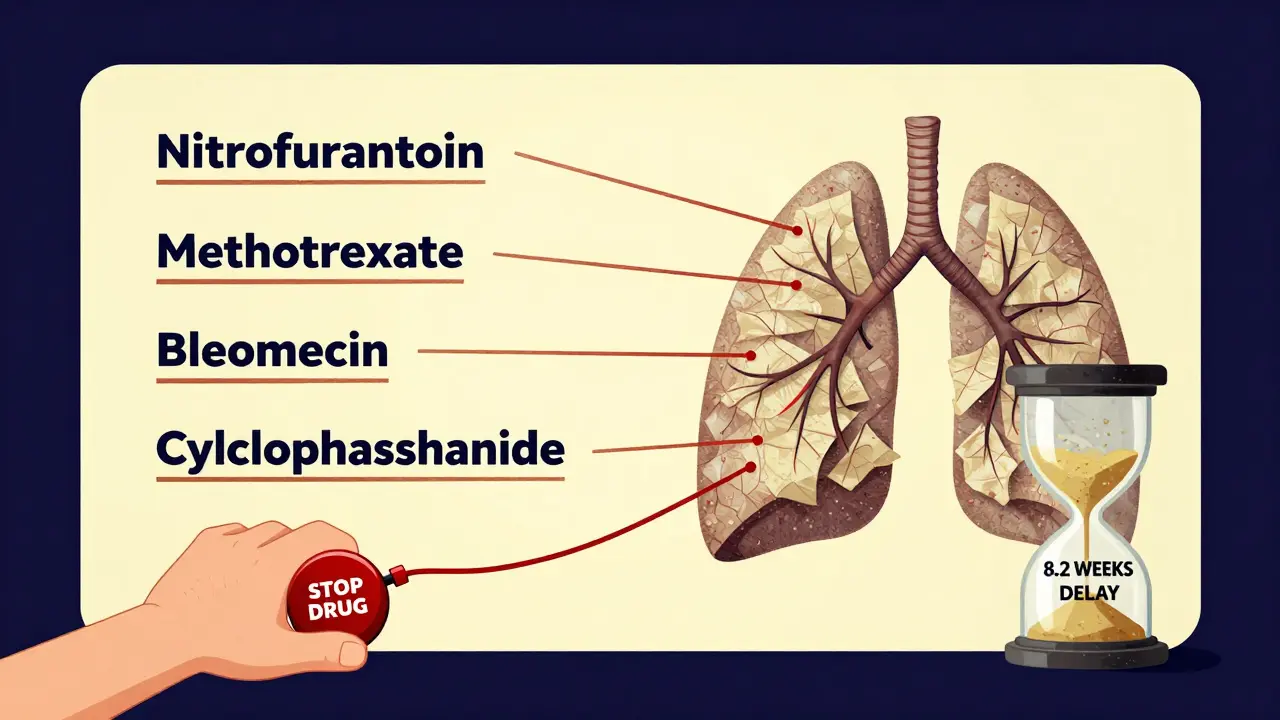
Not every drug causes this. But these five are the most common-and the most dangerous because they’re widely prescribed.- Nitrofurantoin: Used for urinary tract infections, especially in older women. It’s cheap, effective, and often prescribed for months as a preventive. But after 6 months to 10 years of use, it can trigger lung scarring. In New Zealand, it was linked to 47 cases of lung injury between 2014 and 2024-the highest of any drug.
- Methotrexate: A staple for rheumatoid arthritis and psoriasis. It’s a powerful immune suppressor. But in 3-7% of users, it causes acute lung inflammation that turns to fibrosis. Symptoms can show up fast: cough, fever, sudden shortness of breath. Doctors often miss it because they assume it’s pneumonia.
- Amiodarone: Used for irregular heart rhythms. It’s one of the most effective anti-arrhythmics, but it builds up in your body over time. After 400 grams total (about 6-12 months of daily use), the risk spikes. Between 5-7% of long-term users develop lung damage. And once it happens, it can be fatal-even after stopping the drug.
- Bleomycin: A chemotherapy drug. It’s used for testicular cancer and lymphoma. Up to 20% of patients on high doses develop severe lung toxicity. The damage can come on quickly. Many patients don’t survive it.
- Cyclophosphamide: Another chemo drug, used for autoimmune diseases and cancer. About 3-5% of users get lung scarring. The risk increases with higher doses and longer treatment.
These aren’t obscure drugs. They’re in everyday prescriptions. And if you’re on any of them, you should know the signs.
How Do You Know If It’s Your Medicine-or Just Aging?
The symptoms are easy to ignore:- A dry cough that won’t go away
- Getting winded faster than usual-walking to the mailbox, climbing stairs
- Unexplained fatigue
- Fever or joint pain without infection
Most people blame it on getting older. Or they think it’s asthma. Or a cold that won’t quit. But if you’re on one of these drugs and you’re having these symptoms, it’s not normal. It’s a red flag.
Studies show patients wait an average of 8.2 weeks before getting the right diagnosis. By then, the scarring is often advanced. That’s why doctors need to ask: “What meds are you taking?” Not just “Do you smoke?” or “Do you have allergies?”
A 2022 survey found only 58% of primary care doctors routinely ask about lung symptoms in patients on high-risk drugs. That’s not good enough.

Can You Reverse It? Yes-if You Catch It Early
The good news? DIPF is one of the few forms of pulmonary fibrosis that can be stopped-or even reversed-if caught early.Step one: Stop the drug. Immediately. No waiting. No “let’s see how it goes.” If your doctor suspects DIPF, they should stop the medication right away. In 89% of cases, patients improve within three months of stopping the drug.
Step two: Steroids. High-dose prednisone (0.5-1 mg per kg of body weight) is often started to calm the inflammation. It’s not a cure, but it can slow or halt the scarring. Tapering takes 3-6 months. You’ll need close monitoring.
Step three: Oxygen. If your oxygen levels drop below 88% at rest, you’ll need supplemental oxygen. It won’t fix the scarring, but it will keep you alive and more comfortable.
Step four: Monitoring. You’ll need lung function tests-spirometry and diffusion capacity-every 3-6 months. These measure how well your lungs are working. Without them, you won’t know if you’re improving or declining.
Recovery isn’t guaranteed. About 15-25% of patients end up with permanent lung damage. But 75-85% recover well-if they stop the drug in time.
Why This Is Getting Worse
The number of reported cases has jumped 23.7% over the past decade. Why?- More people are taking these drugs. Methotrexate for arthritis, amiodarone for heart rhythm, nitrofurantoin for UTIs-all are used more than ever.
- New drugs are being approved. Immune checkpoint inhibitors for cancer (like Keytruda and Opdivo) are now linked to pulmonary fibrosis. These are powerful, life-saving drugs-but they can also turn the immune system against the lungs.
- We’re getting better at spotting it. More doctors know to look for it. But that also means we’re seeing more cases than before.
And here’s the scary part: There are over 50 medications known to cause this. The list keeps growing. Every new drug that hits the market carries a risk. And for many, we don’t know the full story yet.
What You Should Do Right Now
If you’re taking one of these drugs:- Don’t panic. Most people don’t get this side effect.
- Know the symptoms. Dry cough? Shortness of breath? Unexplained fatigue? Write them down.
- Ask your doctor: “Could this drug affect my lungs?”
- Request a baseline lung function test if you’re starting long-term treatment.
- If you notice symptoms, don’t wait. Go back to your doctor. Say: “I’m on [drug name]. I think this might be drug-induced lung damage.”
If you’re a caregiver for an older adult on long-term meds, pay attention. They might not realize they’re breathing harder. They might think it’s just getting old.
And if you’re a doctor: Ask about meds. Don’t assume. Document. Educate. It could save a life.
What’s Being Done?
Regulators are waking up. In December 2024, New Zealand’s Medsafe issued a public alert about drug-induced lung injury. They reminded doctors to warn patients. They flagged nitrofurantoin, methotrexate, and amiodarone as top culprits.The Pulmonary Fibrosis Foundation launched a physician education program in 2024. Early results show a 32% drop in diagnostic delays in clinics that participated.
Researchers are now hunting for genetic markers that predict who’s at risk. The goal? Before you even start a high-risk drug, a simple blood test could tell you if your lungs are vulnerable.
That’s the future. But right now, awareness is the best tool we have.
Final Reality Check
Medicines save lives. That’s not in question. But they also carry hidden risks. Drug-induced pulmonary fibrosis is one of them. It’s not a fluke. It’s not rare. And it’s not always caught in time.If you’re on a long-term medication-especially for heart, lung, autoimmune, or cancer conditions-know the signs. Ask the questions. Don’t wait for a cough to become a crisis.
Your lungs don’t heal easily. But they can be protected-if you act before the scarring begins.
Hanna Spittel
This is just Big Pharma’s way of keeping us hooked 😒 They know you’ll never stop taking the pills even if your lungs turn to dust. I’ve seen it happen-doctors don’t care. They get paid per script. 💸
John Chapman
I’m so glad someone finally said this. My aunt was on nitrofurantoin for 8 years and no one ever warned her. She’s on oxygen now. Don’t wait until you’re gasping-ask your doctor TODAY. 💪❤️
Urvi Patel
This article is basic but correct. In India we have zero awareness about drug induced fibrosis. Doctors prescribe amiodarone like candy. No tests. No follow up. Just pills. And people die quietly
anggit marga
USA thinks it’s the only country with bad medicine? Try Nigeria where people buy antibiotics off the street and then wonder why they can’t breathe. This isn’t a US problem it’s a global failure
Frank SSS
I read this and thought ‘cool’ then remembered I’m on methotrexate. Guess I’ll just ignore the cough then. 😴
Paul Huppert
This is terrifying but so important. I’ve had a dry cough for months and thought it was allergies. Should I get tested? What’s the first step?
Brady K.
Ah yes, the classic ‘your lungs are dying but your insurance premium is rising’ paradox. We’ve optimized healthcare into a profit-driven death spiral. Congrats, capitalism. 🎉
Kayla Kliphardt
I’m on amiodarone. I didn’t know this was a risk. I’ll call my cardiologist tomorrow. Thanks for the wake-up call.
Joy Nickles
I just read this and I’m so scared I’m gonna die in my sleep!!! I’ve been on methotrexate for 2 years and I’ve had a cough for 6 months and I’m 34 and I don’t want to die and I’m so mad at my doctor for not telling me and why didn’t anyone warn me why why why
Emma Hooper
You know what’s wild? People will take 10 different supplements to ‘detox’ their liver but won’t question a 50-year-old drug that’s literally turning their lungs to parchment. We’re a nation of contradictions wrapped in a placebo.
Martin Viau
The real issue here is systemic underfunding of pulmonology. We’ve got oncologists popping champagne over chemo wins but no one’s tracking lung toxicity metrics. It’s not negligence-it’s institutional neglect.
Marilyn Ferrera
If you're on any of these meds, get a baseline PFT. It takes 15 minutes. Save yourself years of suffering. And if your doctor says ‘it’s unlikely’-ask for a referral. You’re not paranoid. You’re proactive.






Write a comment