Let’s say you’ve been taking a brand-name pill for high blood pressure for years. Your doctor switches you to the generic version. A week later, you feel a little off. Your headache comes back. You start to wonder: Is the generic really the same? You’re not alone. Millions of people feel this way - even though science says it shouldn’t matter.
They’re the Same Medicine - But Your Brain Doesn’t Believe It
Generic drugs aren’t knockoffs. They’re not cheaper imitations. They’re exact copies of brand-name drugs, down to the active ingredient. The U.S. Food and Drug Administration (FDA) requires generics to deliver the same amount of medicine into your bloodstream at the same speed as the brand-name version. The acceptable difference? Between 80% and 125%. That’s not a loophole - it’s a scientifically proven range where no meaningful difference in effect exists for over 95% of medications. Yet, 13% of U.S. adults still believe brand-name drugs work better. Even more - 20% - think generics cause more side effects. Why? Because perception isn’t built on data. It’s built on experience, fear, and stories.The Nocebo Effect: When Expectations Make You Feel Worse
There’s a well-documented psychological phenomenon called the nocebo effect. It’s the opposite of the placebo effect. Instead of feeling better because you believe a treatment works, you feel worse because you believe it won’t. A 2023 study in JAMA Network Open showed this clearly. Patients told their generic pill was "just as effective" had 34% better adherence. Those told it was "less effective" had 41% worse outcomes - even though the pill was identical. Your brain doesn’t need proof. It needs reassurance. If you’re told, "This is the cheap version," your body starts looking for reasons to confirm that. Pharmacists in rural Alabama report patients refusing generics because they believe they’re "for poor people." In urban clinics, patients say their anxiety got worse after switching from brand-name sertraline to the generic - despite identical active ingredients. The drug didn’t change. Their belief did.Why Do Doctors Sometimes Doubt Generics Too?
It’s not just patients. About 11% of physicians believe generics are less effective. Another 27% think they cause more side effects. That’s not because they’re misinformed - it’s because they’ve seen patients react badly after switching. But here’s the catch: those reactions often happen right after the switch. Not because the drug is different - but because the patient is anxious. They notice every little change. A new pill shape. A different color. A slightly different label. Their body, already primed to expect trouble, interprets normal fluctuations as side effects. For drugs with a narrow therapeutic index - like warfarin or levothyroxine - doctors are extra cautious. And rightly so. But even here, decades of data show no consistent difference in outcomes between brand and generic versions. The American College of Clinical Pharmacy confirms: when properly manufactured, generics work just as well.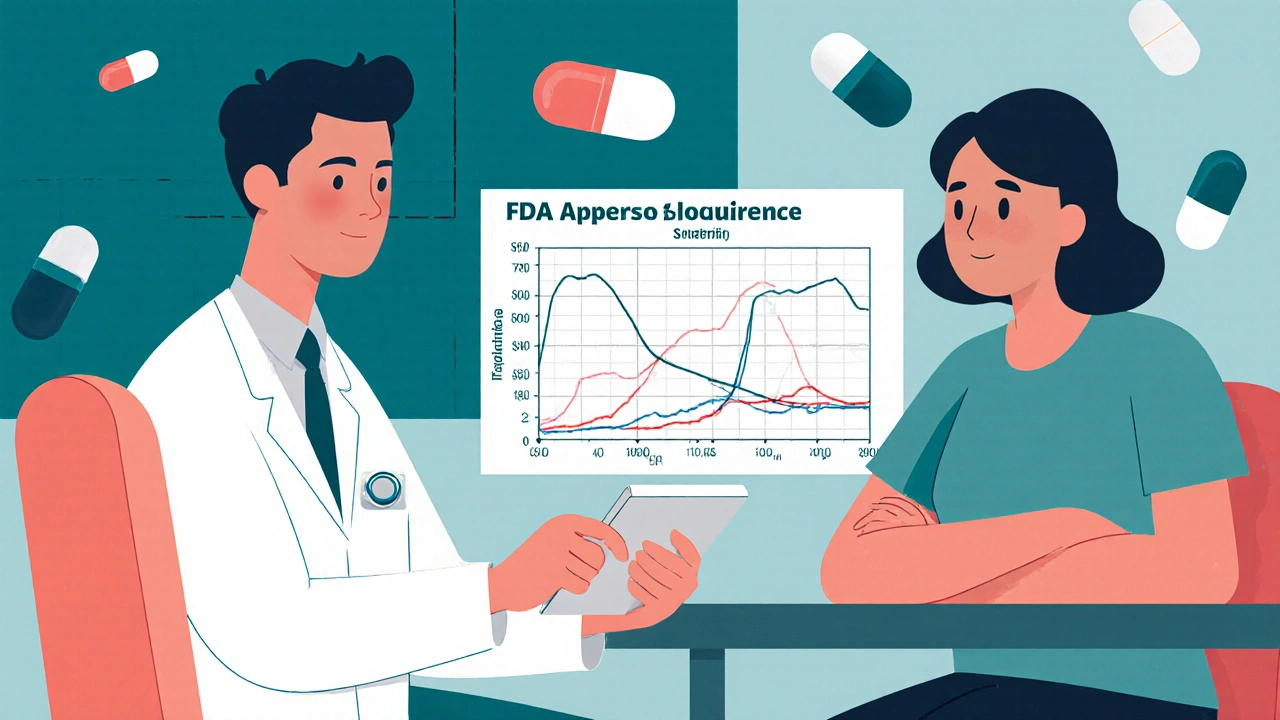
The Cost Difference Is Massive - And It Matters
Brand-name drugs can cost 80-85% more than generics. Since 2009, generics have saved the U.S. healthcare system $1.7 trillion. That’s not a small number. It’s enough to cover millions of prescriptions for people who otherwise wouldn’t be able to afford them. But if patients stop taking their meds because they think the generic doesn’t work, those savings vanish. A 2019 study found 22% of people who believed generics were inferior stopped taking them early. Only 8% of those who didn’t have that belief did. That’s not just a perception gap - it’s a public health risk.Who’s Behind the Doubt?
You’d think the drug companies selling generics would want everyone to trust them. But the real problem? The brand-name companies that still make billions off their old patents. A 2021 investigation by STAT News found brand-name manufacturers spend $1.8 billion a year on marketing campaigns that subtly undermine generics. Ads don’t say, "Generics don’t work." They say, "Your health is too important to risk." Or, "We’ve spent decades perfecting this formula." The message? Your generic is a shortcut. Your life isn’t worth it. These campaigns work. They prey on fear. They make people feel like they’re choosing between safety and savings - when the truth is, they’re choosing between two identical medicines.What Actually Makes a Difference?
The biggest factor in whether someone accepts a generic? What their doctor says. A 2016 study led by Dr. William Shrank showed that when doctors clearly explain, "This is the exact same medicine," patient acceptance jumps dramatically. Showing the patient the FDA’s bioequivalence data helps too. So does simply saying, "I’ve prescribed this generic to hundreds of patients - it works just like the brand." One pharmacist in Chicago told me about a patient who refused her generic thyroid medication for two years. She kept saying, "It doesn’t make me feel right." The pharmacist didn’t argue. He pulled up the FDA website, showed her the list of active ingredients - identical to her brand-name pill. Then he said, "You know what’s different? The filler. The dye. The shape. But not the medicine. That’s the same." She started taking it the next day.
Why Do Some People Still Feel Different?
You might be thinking: "But I felt different on the generic." You’re not imagining it. You felt something. But it’s not because the drug is weaker. It’s because your body is adjusting. Generic pills use different inactive ingredients - the fillers, dyes, and binders that hold the pill together. These don’t affect how the medicine works. But they can change how the pill tastes, how fast it dissolves, or even how it feels in your throat. For some people, that’s enough to trigger a psychological response. Also, if you’ve been on the same brand-name drug for years, your body gets used to it. Switching - even to an identical medicine - can feel like a disruption. That’s normal. It doesn’t mean the new pill is broken.What Should You Do?
If your doctor switches you to a generic:- Ask: "Is the active ingredient the same?" The answer will always be yes.
- Don’t assume a change in how you feel means the drug isn’t working. Give it two to four weeks.
- If symptoms persist, talk to your doctor - but don’t assume it’s the generic’s fault. It might be stress, sleep, diet, or something else.
- Keep taking it. Stopping because you think it’s "less effective" is riskier than staying on it.
The Bigger Picture
Generics aren’t just cheaper. They’re essential. Without them, millions of people couldn’t afford their prescriptions. Chronic disease management - for diabetes, high blood pressure, depression - depends on consistent access. Perception gaps don’t just hurt wallets. They hurt lives. Countries like Canada and the UK have far higher generic acceptance rates - not because their drugs are better, but because their health systems actively educate patients. The FDA’s "It’s the Same Medicine" campaign has reached 27 million people. But only 19% remember it. The fix isn’t more ads. It’s better conversations. Between doctors and patients. Between pharmacists and families. Between you and your own doubts. The science is clear. The data is solid. The medicine is the same. The only thing left to change? What you believe.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence - meaning they deliver the same amount of medicine into your bloodstream at the same rate. The allowed variation is 80-125%, which is scientifically proven to have no meaningful clinical impact for most drugs.
Why do some people feel worse after switching to a generic?
The medicine itself hasn’t changed. But your brain might be reacting to the switch - a phenomenon called the nocebo effect. If you believe the generic is inferior, your body may interpret normal changes - like a different pill shape or filler - as side effects. Anxiety about the switch can also worsen symptoms. Give it 2-4 weeks before deciding it’s not working.
Are generics made in worse facilities?
No. All generic drug manufacturers - whether in the U.S., India, or elsewhere - must follow the same FDA standards for quality and safety (cGMP). While foreign facilities get inspected more often, that’s because there are more of them. The final product must meet the same standards. The FDA tests samples from both brand and generic drugs randomly - and finds no difference in quality.
Can generics cause more side effects?
Not because they’re different drugs. Side effects come from the active ingredient - which is identical. Sometimes, people report more side effects after switching because they expect them. Rarely, differences in inactive ingredients (like dyes or fillers) might cause mild reactions - but these are uncommon and not related to effectiveness.
Should I avoid generics for drugs like thyroid medication or blood thinners?
No. Even for drugs with a narrow therapeutic index - like levothyroxine or warfarin - studies show no consistent difference in outcomes between brand and generic versions. The FDA and the American College of Clinical Pharmacy both confirm they are therapeutically equivalent. If your doctor switches you, monitor your levels as usual - but don’t assume the generic is the problem.
Why do brand-name companies spend so much to discourage generics?
Because generics cut into their profits. Once a patent expires, generics can sell for 80-85% less. Brand-name companies spend billions on marketing that implies their drug is superior - without making false claims. Phrases like "trusted for decades" or "developed with precision" subtly suggest generics are inferior. It’s not about safety - it’s about market share.
How can I be sure my generic is safe?
Check the FDA’s website for the drug’s approval status. All approved generics are listed. Ask your pharmacist for the manufacturer’s name - most are reputable companies with decades of experience. If your pill looks different, that’s normal. The active ingredient hasn’t changed. If you’re still unsure, ask your doctor to verify the bioequivalence data.
Barry Sanders
This is why people are dumb. You switch to generic, feel weird, and immediately blame the pill. Not your stress, not your sleep, not your coffee intake-nope, it’s the damn generic. The science is clear, but your brain’s a conspiracy theorist with a pharmacy receipt.
kshitij pandey
Bro, I live in India, generics are life here. My mom takes blood pressure medicine for 15 years-half the price, same results. Doctors here don’t even say ‘generic,’ they just say ‘medicine.’ No drama, just health. 💪
Brittany C
There’s a fascinating interplay between pharmacokinetics and cognitive bias here. The nocebo effect is a well-documented confounder in therapeutic adherence studies, particularly in populations with low health literacy. The FDA’s bioequivalence thresholds are statistically robust-yet perceptual dissonance overrides evidence-based decision-making at the individual level.
Sean Evans
LOL you people are so gullible. Brand-name companies are literally paying people to lie to you. They don’t care if you die-they care if you keep buying their $200 pills. I switched to generic levothyroxine and my TSH dropped to perfect levels. But nooo, you’d rather believe the pharma ads than your own lab results. 🤡
Anjan Patel
Let me tell you something, my friend. In my village, people say, 'If it's cheap, it's trash.' They won't take generics even if their heart is failing. Why? Because they think the rich man's pill has magic in it. I told my cousin, 'The active ingredient is the same!' He said, 'But the box looks different!' That's not science-that's superstition wrapped in a prescription bottle.
Scarlett Walker
My doctor switched me to generic sertraline and I freaked out for a week. I thought I was going back into a depression spiral. But I stuck with it, gave it 3 weeks, and honestly? I feel better than I have in years. The pill’s the same. My brain was just being dramatic. 😅
Hrudananda Rath
It is a matter of profound intellectual dissonance that the populace continues to ascribe differential efficacy to pharmaceutical agents based upon branding, when the chemical moiety, bioavailability profile, and pharmacodynamic parameters are statistically indistinguishable. The pharmaceutical industry’s marketing apparatus has successfully weaponized consumer psychology against evidence-based medicine. This is not merely a failure of education-it is a systemic collapse of rationality.
Brian Bell
Same here. I switched to generic blood pressure med and thought I was gonna die. Turned out I was just stressed about the switch. Now I’m like, ‘yo, why did I even care?’ 🤷♂️




Write a comment