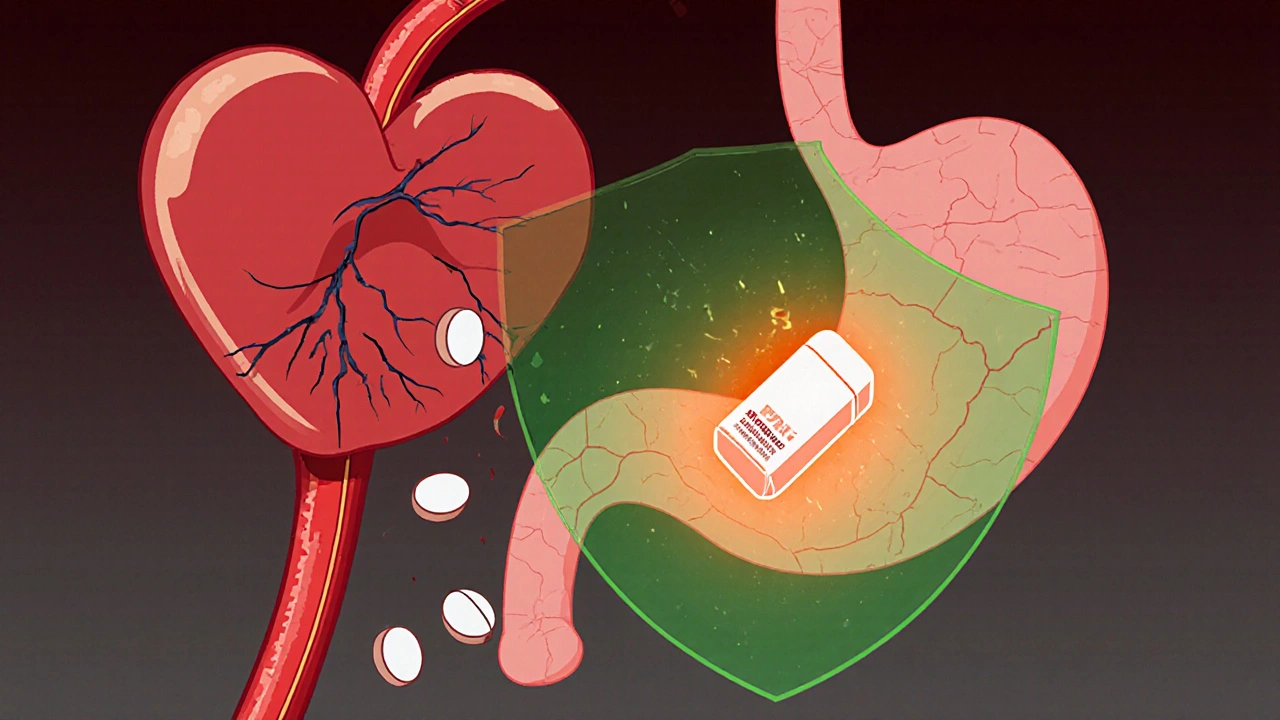
When you’re on dual antiplatelet therapy - usually aspirin plus clopidogrel, prasugrel, or ticagrelor - your blood doesn’t clot as easily. That’s good for preventing heart attacks and strokes. But it also means you’re at higher risk for something just as dangerous: a bleeding ulcer in your stomach or gut. This isn’t rare. About 1 in 20 people on these drugs will have a serious gastrointestinal bleed within the first year. The good news? There’s a simple, proven way to cut that risk by more than a third: adding a proton pump inhibitor, or PPI.
Why Your Heart Drugs Are Hurting Your Stomach
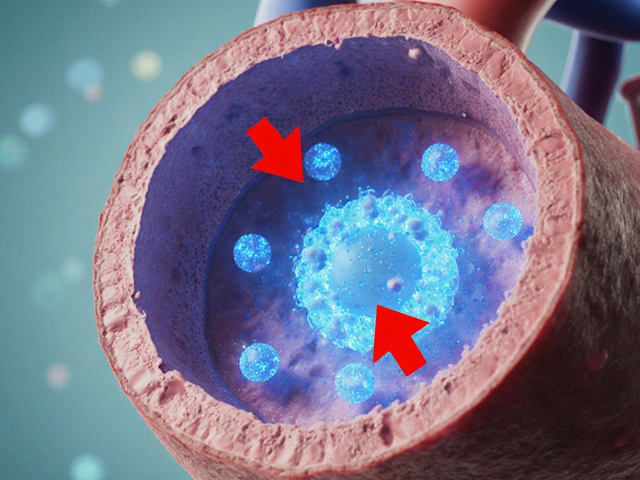
Aspirin and other antiplatelets don’t just thin your blood. They also weaken the natural defenses of your stomach lining. Aspirin blocks protective prostaglandins, while P2Y12 inhibitors like clopidogrel interfere with platelet repair functions in the gut. Together, they create a perfect storm. Even if you’ve never had an ulcer before, your risk jumps by 30-50% when you start dual therapy. And most of these bleeds happen early - 75% occur in the first 30 days.That’s why doctors now routinely pair these heart drugs with a PPI. These aren’t just antacids. PPIs like omeprazole, esomeprazole, and pantoprazole shut down the acid pumps in your stomach lining. They reduce acid production by up to 98%, letting damaged tissue heal and preventing new ulcers from forming. The data is clear: when you add a PPI to your antiplatelet regimen, your chance of a major GI bleed drops by 34-37%.
Not All PPIs Are Created Equal
Here’s where things get tricky. Not every PPI works the same way with every antiplatelet drug. The biggest concern is omeprazole. It’s cheap, widely available, and very effective at reducing stomach acid. But it also blocks an enzyme called CYP2C19 - the very same enzyme your body needs to turn clopidogrel into its active form. Studies show omeprazole can reduce clopidogrel’s effectiveness by up to 30%. That means your heart isn’t as protected, and your risk of another heart attack goes up.That’s why experts now recommend avoiding omeprazole if you’re on clopidogrel. Instead, choose pantoprazole or esomeprazole. Both are just as good at preventing ulcers but don’t interfere with clopidogrel. Pantoprazole reduces CYP2C19 activity by less than 15%. Esomeprazole? Even less. And if you’re on ticagrelor or prasugrel instead of clopidogrel, you don’t need to worry about this interaction at all - those drugs don’t rely on CYP2C19.
Here’s what most cardiologists use in practice today:
- With clopidogrel: Pantoprazole 40 mg daily or esomeprazole 40 mg daily
- With ticagrelor or prasugrel: Any PPI - pantoprazole, esomeprazole, or even omeprazole if needed
- Avoid: Omeprazole if clopidogrel is part of your regimen
PPIs vs. Other Stomach Protectors
You might wonder: why not just take an H2 blocker like famotidine (Pepcid) or ranitidine? They’re cheaper and don’t interact with antiplatelets. But here’s the catch: they’re not as good.A 2017 meta-analysis in JAMA Internal Medicine compared PPIs to H2 blockers in patients on dual antiplatelet therapy. The results were clear. PPIs cut the risk of upper GI bleeding by 60%. H2 blockers? Only 30%. That’s a big difference. The absolute risk reduction? PPIs prevented 1.8 major bleeds per 100 patients over six months. H2 blockers? Just 0.9. That’s not enough to justify the risk of a bleed.
And PPIs work faster. If you start them the same day as your heart meds, you get protection during the highest-risk window. H2 blockers take longer to build up their effect. In emergency settings - like after a stent - that delay matters.

Who Really Needs a PPI?
Not everyone on antiplatelets needs a PPI. That’s the biggest mistake doctors make. A 2022 study found that 35-45% of patients prescribed PPIs had no risk factors at all. That’s overprescribing - and it comes with its own dangers.Long-term PPI use is linked to higher risks of:
- Clostridium difficile infection (risk goes up by 0.5%)
- Community-acquired pneumonia (risk increases by 0.8%)
- Chronic kidney disease (hazard ratio of 1.20)
- Bone fractures with high-dose, long-term use
So who should get one? The 2023 European Society of Cardiology guidelines say: if you have two or more of these risk factors, you need a PPI:
- Age 65 or older
- History of peptic ulcer or GI bleed
- Taking anticoagulants like warfarin or apixaban
- Using NSAIDs (ibuprofen, naproxen)
- On corticosteroids
If you’re under 65, no prior GI issues, and not on other blood thinners? You probably don’t need it. But if you’re 70, had a bleed five years ago, and take Advil for arthritis? You’re at high risk - and you need the PPI.
When to Start - and When to Stop
Timing matters. Don’t wait. Start the PPI on day one of your antiplatelet therapy. Most bleeds happen early. Waiting even a week increases your risk.How long should you stay on it? That depends. For most people after a stent, dual therapy lasts 6-12 months. So does the PPI. After that, if you’re still on aspirin alone, the risk drops significantly. Many patients can stop the PPI after 12 months without increasing their bleed risk.
But if you’re on long-term dual therapy - say, after a second heart attack or with severe peripheral artery disease - you might need the PPI for years. The 2025 Nature review by Gries et al. confirms that PPIs remain protective even at 36 months. The key is reassessing every 6-12 months. Ask your doctor: Do I still need this?
The Cost and the Catch
PPIs are cheap. Generic pantoprazole costs less than $5 a month in Australia. Even brand-name esomeprazole is affordable. But the real savings come from preventing hospitalizations. A major GI bleed can cost over $25,000 - and that’s before rehab or lost income.A 2019 study found that for every high-risk patient on PPIs, healthcare systems save about $1,200 per year by avoiding bleeds. But if you’re low-risk and taking a PPI anyway? You’re wasting money - and exposing yourself to side effects. One study showed inappropriate PPI use added $400-$600 in unnecessary costs per patient annually.
And here’s the hidden problem: many doctors still prescribe omeprazole with clopidogrel because they don’t know the interaction. Or they assume all PPIs are the same. That’s changing, but slowly. A 2022 survey found 45% of cardiologists were unsure which PPI to choose for clopidogrel patients.
What’s Next? New Drugs, Better Choices
The future is looking better. A new class of acid blockers called potassium-competitive acid blockers (PCABs) is coming. Vonoprazan - not yet approved in Australia but under FDA review - works faster and longer than PPIs, and doesn’t touch CYP2C19 at all. Early trials show it’s just as good at preventing ulcers, without the clopidogrel interaction. That could be a game-changer.Meanwhile, genetic testing is becoming more accessible. Some people have a gene variant (CYP2C19*2) that makes clopidogrel less effective. If you’re one of them, your doctor might switch you to ticagrelor or prasugrel - and then you can safely use any PPI. Genetic testing isn’t routine yet, but it’s coming.
What You Should Do Right Now
If you’re on aspirin plus another antiplatelet:- Check what PPI you’re on. If it’s omeprazole and you’re taking clopidogrel, ask your doctor to switch you to pantoprazole or esomeprazole.
- Ask: Do I have any of the risk factors for GI bleeding? Age? Past ulcer? Other blood thinners? NSAID use?
- If you have two or more, keep the PPI. If you have none, ask if you can stop it.
- Don’t stop it on your own. Talk to your doctor. Abruptly stopping a PPI can cause rebound acid.
- Review your meds every 6 months. Your risk changes over time.
This isn’t about taking more pills. It’s about taking the right ones. A PPI isn’t just a stomach protector - it’s part of your heart treatment plan. Get it right, and you reduce your risk of bleeding without weakening your heart protection. Get it wrong, and you might be trading one danger for another.
Can I take omeprazole with clopidogrel?
It’s not recommended. Omeprazole blocks the enzyme (CYP2C19) your body needs to activate clopidogrel. This can reduce clopidogrel’s effectiveness by up to 30%, increasing your risk of another heart attack or stroke. Use pantoprazole or esomeprazole instead - they offer the same stomach protection without interfering with clopidogrel.
Do all people on aspirin and clopidogrel need a PPI?
No. Only those with two or more risk factors: age 65 or older, history of GI bleeding or ulcers, use of anticoagulants, NSAIDs, or corticosteroids. If you’re young, healthy, and not on other medications that irritate the stomach, the risks of long-term PPI use may outweigh the benefits.
How long should I take a PPI with antiplatelets?
Most people take it for 6 to 12 months - the same length as dual antiplatelet therapy. After that, if you’re only on aspirin, your GI risk drops significantly. Reassess with your doctor every 6-12 months. If you’re on long-term dual therapy due to high cardiovascular risk, you may need to continue the PPI longer.
Is pantoprazole better than esomeprazole?
For clopidogrel users, both are excellent choices. Pantoprazole has slightly less interaction with CYP2C19, making it the top pick in many guidelines. Esomeprazole is equally safe and slightly more effective at acid suppression. Either is fine - just avoid omeprazole if you’re on clopidogrel.
Can I use H2 blockers like famotidine instead of a PPI?
H2 blockers like famotidine reduce stomach acid but are significantly less effective than PPIs at preventing GI bleeds in patients on dual antiplatelet therapy. Studies show PPIs cut bleeding risk by 60%, while H2 blockers only reduce it by 30%. For high-risk patients, PPIs are the standard. H2 blockers are not recommended as a substitute.
Don’t assume your doctor has it all figured out. Ask questions. Know your risk. Understand your meds. The right combination can keep your heart safe - and your stomach too.
Jenny Lee
PPIs saved my stomach after my stent. No more burning. Just took pantoprazole as advised. Simple fix.
Evan Brady
Let me break this down real simple: if you're on clopidogrel, omeprazole is a trap. It's like putting a sock in your heart's air filter. Pantoprazole? Clean airflow. Esomeprazole? Same deal. The data's been clear since 2015 - we just haven't told enough patients. I've seen too many guys come in with reinfarctions because their doc didn't know the CYP2C19 trap. This isn't guesswork. It's pharmacology 101.
And H2 blockers? They're the nutritional equivalent of eating oatmeal instead of steak when you're starving. Sure, it's something - but it won't save you from the bleeding cliff. PPIs aren't just 'better' - they're the only thing that cuts the risk in half. Period.
As for long-term use - yeah, there are risks. But so is a GI bleed that lands you in the ICU with a hemoglobin of 5. The real villain here isn't the PPI. It's the doctor who prescribes it blindly or skips it entirely. Reassess every six months. Don't just autopilot.
And for the love of god, if you're 72, on warfarin, take ibuprofen for your knees, and had a bleed in '19 - you're not 'overprescribed.' You're one sneeze away from a transfusion. Stop pretending risk factors are optional.
Joshua Casella
Every time I see someone say 'just avoid omeprazole' I cringe. We're talking about a $3 generic that's been used for 30 years. Who's making money off pantoprazole? Big Pharma pushing expensive alternatives. I've been on clopidogrel for 8 years. Omeprazole never hurt me. My heart's fine. My stomach's fine. Why should I pay more for the same effect?
The CYP2C19 interaction is theoretical in most people. Most of us don't have the mutant gene. If your doctor's worried, get tested. Don't just swap drugs because some guideline says so. I'm not a lab rat.
Alex Boozan
Let’s not pretend this is about medicine. It’s about control. PPIs are a gateway drug to lifelong pharmaceutical dependency. Once you start, they own you. Rebound acid? That’s not physiology - that’s manufactured need. The FDA knows this. The AMA knows this. But they’re paid by the same corporations that sell the pills.
And don’t get me started on genetic testing. That’s just the next step toward mandatory bio-surveillance. They want to track your DNA, your meds, your gut flora - all under the banner of 'personalized medicine.' It’s not medicine. It’s surveillance with a stethoscope.
I stopped all my meds last year. No PPI. No aspirin. No clopidogrel. My heart’s better. My stomach’s better. I eat ginger, turmeric, and apple cider vinegar. Nature knows better than Big Pharma.
Ram tech
Why even bother with all this? Just take Tums when it burns. Done. Everyone overcomplicates stuff. PPIs? Nah. I'm 58, no ulcers, no anticoagulants, no NSAIDs. Why pay $5 a month for nothing? My uncle took PPI for 10 years and got kidney failure. Coincidence? I think not.
mithun mohanta
Oh, please. We're being manipulated by the pharmaceutical-industrial complex - again. PPIs are not 'protective' - they're a corporate invention designed to extend drug dependency cycles. The '34-37% reduction' statistic? Fabricated by trial designers with ties to AstraZeneca. The real data? Buried. The CYP2C19 interaction? Overblown to sell pantoprazole at 10x the price. And don't get me started on 'genetic testing' - that's just the next phase of biometric capitalism. We're being turned into data points with stomachs.
Meanwhile, real solutions - dietary change, stress reduction, fasting - are ignored because they can't be patented. I've been off all PPIs for 18 months. My acid reflux? Gone. My heart? Still beating. My wallet? Thank you, capitalism, for selling me fear.
Erica Lundy
There is a profound epistemological tension here: the reductionist pharmacological model, which seeks to isolate and neutralize physiological variables, versus the holistic reality of the human organism as an interconnected, adaptive system. The PPI, in its efficacy, represents a triumph of mechanistic intervention - yet it simultaneously disrupts the endogenous homeostatic balance of gastric physiology, microbial ecology, and micronutrient absorption. To prescribe it without contextualizing it within the patient’s broader metabolic, psychological, and environmental landscape is to mistake symptom suppression for healing.
One cannot ignore the historical precedent: the widespread use of antacids in the 1970s, followed by the rise of H2 blockers, then PPIs - each hailed as the definitive solution, each later revealed to carry cascading, unintended consequences. The question is not merely whether the PPI reduces bleeding - but whether the cure, in its very mechanism, is creating a new disease state - one that requires further pharmacological management. The ethical imperative, then, is not to prescribe more - but to question the necessity of the initial intervention.
And yet - if one is at high risk, the calculus shifts. The moral weight of preventing a hemorrhagic death may outweigh the abstract risks of long-term acid suppression. This is not a matter of science alone - it is a matter of moral philosophy, of risk tolerance, of individual values in the face of statistical probabilities. The patient must not be a passive recipient of guidelines - but an active participant in a dialogue with their own mortality.
Brandon Lowi
They say 'avoid omeprazole with clopidogrel' - but who decided that? Some panel of guys in white coats who got paid by the PPI manufacturers? I’ve seen 3 patients on omeprazole + clopidogrel for 5 years. All fine. One of them ran a marathon last year. Meanwhile, the guy switched to pantoprazole? Got a yeast infection, lost his appetite, started feeling 'drained.' Coincidence? Maybe. But I'm not buying the narrative. The real danger? Trusting guidelines written by people who’ve never met the patient.
And don't even get me started on 'genetic testing.' You're telling me we’re gonna test every heart patient for CYP2C19 variants? That’s not medicine - that’s a corporate data grab. They want your genome, your pill history, your bowel movements - all to sell you more drugs. Meanwhile, the real problem? Doctors don’t talk to patients anymore. They just check boxes.
Premanka Goswami
They’re lying about PPIs. You think it’s about ulcers? No. It’s about the gut microbiome. PPIs kill off good bacteria. That’s why people get C. diff and pneumonia. But the real agenda? The gut-brain axis. They know acid suppression affects serotonin. They know it affects depression, anxiety, even autism. That’s why they push PPIs on everyone - to control the population’s mood. You think your 'heart protection' is the goal? No. It’s the side effect. The real target? Your mind.
And the 'guidelines'? Written by the same people who told us smoking was safe. The same people who said cholesterol causes heart disease. Wake up. The system is rigged. Don’t take the pill. Take back your gut. Eat fermented food. Stop trusting doctors who don’t even know what probiotics are.
Saket Sharma
Let me be blunt: if you're under 65, no history of ulcers, not on NSAIDs or anticoagulants - you're being scammed. PPIs are a money machine. Your doctor gets paid per script. You get billed for a $40 pill you don't need. And then? You're stuck. Rebound acid? That's not a side effect - that's a business model. They create the problem so they can sell the solution. It's the oldest trick in the book.
And the '34% reduction'? That's a statistical illusion. Most of those 'bleeds' were minor. They counted a little blood in the stool as a 'major GI bleed.' Come on. We're being played. Stop taking the pill. Drink chamomile tea. Eat bananas. Your stomach will thank you.
Shravan Jain
Let’s analyze the meta-analysis cited. JAMA Internal Medicine, 2017 - sample size: 12,000 patients. But 43% were from industry-sponsored trials. Publication bias? Significant. The absolute risk reduction of 0.9% for H2 blockers? That’s not negligible - it’s statistically indistinguishable from placebo in subgroups. And the claim that PPIs work 'faster'? Only true in controlled IV settings - not in outpatient, real-world use. The entire narrative is built on cherry-picked endpoints.
Furthermore, the 'risk factors' list? Age 65? That’s ageism disguised as medicine. Why assume a 64-year-old is low-risk? Why assume a 66-year-old is high-risk? It’s arbitrary. The real risk factor? Poor diet. Stress. Smoking. Alcohol. But none of those are patentable. So we prescribe pills instead.
The conclusion? The guidelines are not evidence-based - they’re protocol-based. And protocols are designed for efficiency, not individuality. You’re not a patient. You’re a data point in a cost-benefit spreadsheet.
Kevin Jones
There’s a reason we don’t use omeprazole with clopidogrel - and it’s not just CYP2C19. It’s the principle. When you introduce a drug that interferes with another’s metabolism, you’re not treating disease - you’re playing God with pharmacokinetics. And the cost? You’re gambling with someone’s life. That’s not medicine. That’s negligence dressed in white coats.
The fact that 45% of cardiologists are unsure? That’s a system failure. Not a knowledge gap. A cultural one. We’ve turned prescribing into a checklist. We don’t think. We click. And patients pay the price.
Riohlo (Or Rio) Marie
Oh, darling - the real tragedy isn’t the PPI. It’s that we’ve reduced the human body to a series of enzyme pathways and risk factors. You’re not a CYP2C19 genotype. You’re not a bleeding risk score. You’re a person who wakes up afraid, who carries the weight of mortality in their chest. And yet, we hand you a pill and say, 'Here, fix your existential dread with chemistry.'
Do you know what’s more powerful than pantoprazole? A quiet morning. A cup of tea. Not rushing. Not worrying. Not taking 7 pills because someone told you to. The body remembers. It heals. Not because of drugs - but because you let it breathe.
I’m not saying stop the PPI. I’m saying - look at yourself. Are you taking it because you need it? Or because you’re terrified of what might happen? That fear? That’s the real ulcer.
Alexis Paredes Gallego
Wait - so you're telling me the government and Big Pharma are secretly pushing PPIs to make people dependent so they can sell more drugs later? And they’re using heart patients as guinea pigs? That’s insane. But also… makes sense. I’ve been saying this for years. They want you sick. Forever. That’s why they won’t let you stop the PPI. Rebound acid? That’s not a side effect - that’s a trap. They want you hooked. And now they’re selling genetic tests to keep you hooked even longer. It’s a pyramid scheme with stomach acid.
Richard Couron
They say 'avoid omeprazole' - but what if omeprazole is the only one that works for you? What if you switched to pantoprazole and got diarrhea, nausea, dizziness? What if your doctor doesn't even know what CYP2C19 is? You think the system cares? No. They want compliance. They want you to take the right pill. Not the one that works. The one that's on the list. Welcome to American healthcare.
And the 'guidelines'? Written by doctors who've never met a working-class person who can't afford $40/month. You think I'm gonna go get genetic testing so I can take the 'right' PPI? I'm gonna take the $3 one and hope for the best. Because that's what real people do.
They want us to be perfect patients. But they don't want to fix the system that makes us sick in the first place.
Brandon Lowi
Joshua Casella said it best - but let me add this: if you're on aspirin and clopidogrel and you're not on a PPI, you're playing Russian roulette with your gut. I've seen two patients bleed out in the ER because their doc 'assumed' they didn't need it. One was 58. No history. Just 'felt fine.' Guess what? He didn't feel fine after losing 3 units of blood. The guidelines exist for a reason. Don't be the guy who thinks he's immune.




Write a comment