Lipid‑Lowering Drugs: What They Are and Why They Matter
If your doctor mentioned a prescription to lower cholesterol, they’re talking about lipid‑lowering drugs. These meds help keep the fat in your blood (called lipids) at healthy levels, which reduces the risk of heart attacks and strokes. Most people take them because lifestyle changes alone haven’t moved the numbers enough.
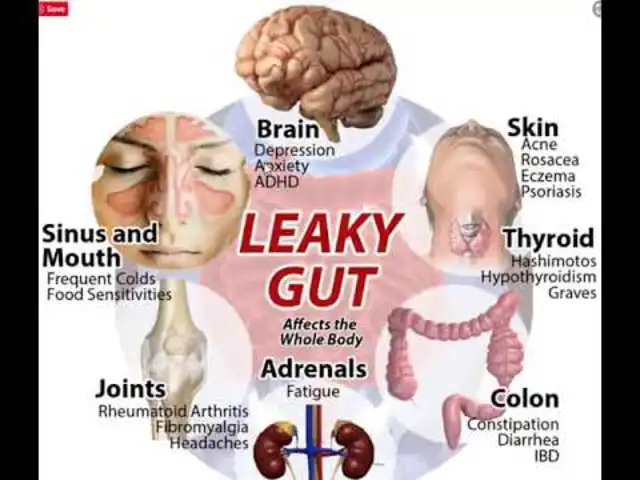
Before you start, know that not every drug works the same way. Some block the liver from making cholesterol, others clean up extra fats, and a few target specific proteins that keep cholesterol from building up in arteries. Picking the right one depends on your blood test results, other health conditions, and how your body reacts.
Common Types of Lipid‑Lowering Drugs
Statins are the most widely prescribed. They lower “bad” LDL cholesterol by stopping the liver’s production line. Popular brands include atorvastatin, simvastatin, and rosuvastatin. Most people see a 20‑50% drop in LDL within a few weeks.
Fibrates (like fenofibrate and gemfibrozil) work better on triglycerides, another type of fat that can raise heart risk when it’s high. They also raise “good” HDL cholesterol a bit.
PCSK9 inhibitors are newer, injectable drugs such as alirocumab and evolocumab. They’re for people who can’t reach target LDL levels with statins alone, or who have genetic conditions that cause very high cholesterol.
Niacin (vitamin B3) can lower LDL and raise HDL, but it often causes flushing and is used less often now.
Each class has its own set of pros and cons, so talk with your doctor about which one fits your profile.
How to Take Them Safely
Start by confirming the dose your doctor wrote. Don’t guess or adjust on your own. Most statins are taken once a day, usually in the evening because the liver works hardest at night.
Eat a balanced diet and avoid heavy alcohol if you’re on fibrates or niacin – it can increase side‑effect risk. Staying hydrated helps your kidneys clear the medication properly.
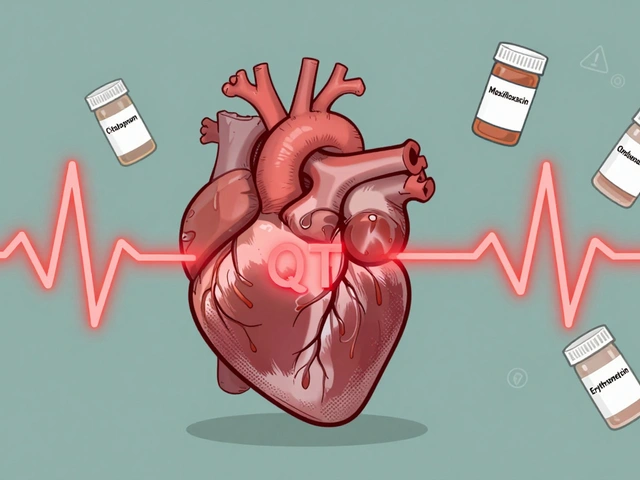
Watch for common side effects: muscle aches, mild stomach upset, or a slight increase in blood sugar. If you feel severe muscle pain, dark urine, or unexplained fatigue, call your doctor right away.
Regular blood tests are a must. Your doctor will check liver enzymes and muscle enzymes (CK) after a month or two, then periodically after that. These tests catch problems before they become serious.
Don’t mix these meds with certain over‑the‑counter products without checking first. For example, grapefruit juice can boost statin levels and raise the chance of side effects.
If you’re pregnant, planning a pregnancy, or breastfeeding, most lipid‑lowering drugs aren’t safe. Discuss alternatives with your doctor.
Finally, remember that meds are just one piece of the puzzle. Pair them with a heart‑healthy diet, regular exercise, and weight control for the best results.
Bottom line: lipid‑lowering drugs can be powerful tools to protect your heart, but they work best when you follow the prescription, keep up with check‑ups, and maintain a healthy lifestyle.
Ezetimibe vs Statins: Benefits, Mechanisms, and Smart Patient Choices
Curious about the buzz around ezetimibe and how it stacks up against statins? This detailed read untangles how ezetimibe blocks cholesterol absorption, breaks down the key outcome data you should care about, and uncovers when your doctor might reach for ezetimibe instead of—or alongside—statins. Dive in to learn who benefits, why outcome studies matter, and how to make sense of the latest cholesterol-lowering strategies. Get the real facts you won’t pick up from a quick doc visit.