
Why Antibiotic Stewardship Matters at Home
The Centers for Disease Control and Prevention (CDC) defines antibiotic stewardship as "the effort to measure and improve how antibiotics are prescribed by clinicians and used by patients." While hospitals have formal programs, home settings account for 30% of all antibiotic use in the U.S. but lack structured guidance. This gap matters because incomplete courses and improper disposal directly feed the rise of drug-resistant infections. Consider this: stopping antibiotics early leaves some bacteria alive, which can mutate and become resistant. The Infectious Diseases Society of America (IDSA) states that incomplete courses increase resistance risk by 23-37% based on studies from 2010-2015. And it’s not just about your health-improper disposal contributes to antibiotic residues in waterways, with 63% of U.S. waterways near populated areas showing detectable levels.
Completing Your Antibiotic Course: What You Need to Know
It’s common to feel better before finishing a prescription. But that’s exactly when bacteria are still fighting back. Here’s the hard truth: stopping early can lead to relapse or create superbugs. The CDC’s Nursing Home Stewardship Guide (2023) explicitly says: "Stopping antibiotics too early can leave some bacteria alive, potentially leading to a relapse or drug resistance." For seniors, who make up 34% of home antibiotic users, this risk is even higher. AARP’s 2023 survey found 38% of seniors don’t complete their courses. How do you avoid this? Set precise reminders. Use pill organizers with alarms or apps like Medisafe (rated 4.7/5 by over 14,000 users). Devices like Hero ($299 upfront, $25/month) automatically dispense doses and track compliance. The key is consistency-taking antibiotics at the exact intervals prescribed, whether every 8 or 12 hours.

Proper Disposal: Don’t Flush or Save Leftovers
Many people keep unused antibiotics "just in case"-but this is dangerous. The Food and Drug Administration (FDA)’s 2022 guidance says never to share antibiotics or reuse old prescriptions. Instead, follow safe disposal steps: mix unused pills with coffee grounds or cat litter to make them unappealing, then seal them in a bag before throwing them in the trash. Never flush them down the toilet or sink. Why? Because flushing contaminates water systems. A CDC survey found only 29% of home users know proper disposal methods, while 61% admit to keeping leftovers. AALLCare’s 2024 guidelines stress that "leftover antibiotics should never be saved for future use" due to risks of incorrect dosing or resistance. If you’re unsure, check local pharmacy take-back programs-some offer free disposal services.
Common Mistakes and How to Avoid Them
Here’s what goes wrong in home settings: sharing antibiotics with family members, skipping doses when feeling better, or using old prescriptions for new symptoms. These actions directly contribute to resistance. For example, using leftover antibiotics for a new infection without consulting a doctor can lead to ineffective treatment. The CDC reports home settings account for 55% of all inappropriate antibiotic use. To avoid this:
- Never share antibiotics-even if symptoms match.
- Complete the full course even if you feel better.
- Dispose of leftovers properly, don’t save them.
- Ask your doctor if antibiotics are truly needed before starting.

Real-Life Challenges and Solutions
Caregivers often struggle with complex schedules. On Reddit’s r/HomeCare subreddit, 68% of users reported difficulties managing doses for seniors taking multiple medications. "My mother takes 7 medications; remembering which antibiotic dose to give at 2am is impossible without a system," wrote one user in October 2023. Solutions like Medisafe or Hero help-42% of successful caregivers use pill organizers with alarms. For antibiotic timeouts (re-evaluating treatment after 48-72 hours), the CDC recommends contacting your doctor if symptoms don’t improve. Facilities using this practice reduced unnecessary antibiotic days by 19.3%, according to the 2022 Stewardship Impact Report. Most home care agencies lack formal protocols, but simple steps like tracking doses in a notebook can make a difference.
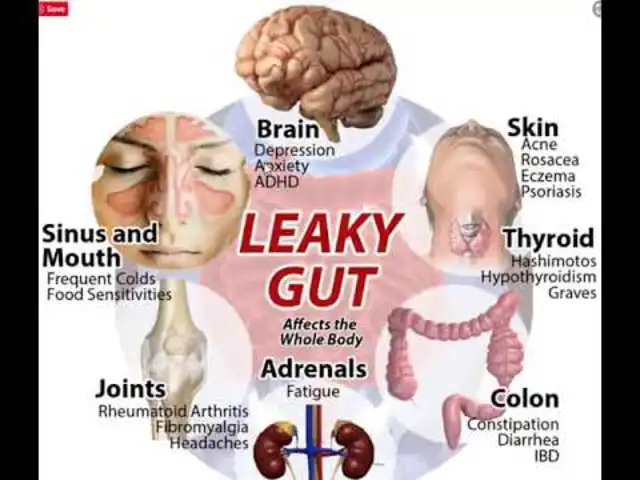
Environmental Impact and Long-Term Risks
Improper disposal doesn’t just affect humans-it harms ecosystems. A 2022 study found antibiotic residues in 63% of U.S. waterways near population centers. These residues create "hotspots" where bacteria develop resistance, eventually spreading to hospitals and communities. The IDSA President, Dr. Helen Boucher, emphasized in the 2023 report that "improper disposal of antibiotics contributes directly to environmental resistance development." Meanwhile, incomplete courses in home settings drive 38% of senior antibiotic non-compliance, leading to 22% higher readmission rates. The FDA’s 2024 National Action Plan aims to reduce inappropriate antibiotic use in community settings by 15% by 2027 through better education. Every step you take at home protects future generations.
What happens if I stop taking antibiotics early?
Stopping early leaves surviving bacteria that can multiply and develop resistance. This makes future infections harder to treat. Studies show incomplete courses increase resistance risk by 23-37% and raise relapse chances by 18.7%.
Can I share my antibiotics with someone else?
Never share antibiotics. What works for one infection might not work for another, and it can cause dangerous side effects or resistance. The FDA explicitly bans this practice.
How should I dispose of unused antibiotics?
Mix pills with coffee grounds or cat litter in a sealed bag before throwing in the trash. Never flush them. Check local pharmacy take-back programs-they often offer free disposal. The CDC confirms this method prevents water contamination.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s close to the next dose. Never double up. If unsure, call your doctor. Apps like Medisafe send reminders to avoid missed doses.
Are there apps to help track antibiotic doses?
Yes! Medisafe (4.7/5 rating) and Hero (automatic dispenser) are top choices. They send reminders, track adherence, and sync with doctors. AALLCare’s 2024 guidelines recommend these tools for seniors.
Why does antibiotic resistance matter to me?
Resistant infections are harder to treat and cost more. They can turn simple cuts into life-threatening situations. The CDC warns that 35,000 U.S. deaths each year stem from resistant bacteria. Your actions at home directly impact this crisis.
Jennifer Aronson
Antibiotic stewardship is a critical public health issue. The CDC reports that 30% of antibiotic use occurs at home, yet there's no structured guidance. Incomplete courses and improper disposal directly contribute to resistance. I've always made sure to complete my prescriptions and dispose of leftovers properly.
Kate Gile
I agree completely. Using pill organizers with alarms has been a game-changer for me. It's easy to forget doses, but having a system in place ensures I take them correctly. Small steps like this really do help prevent resistance.
Gregory Rodriguez
Oh sure, 'complete the course'-because that's what everyone does. Meanwhile, doctors keep prescribing antibiotics for viral infections. The real problem is overprescribing, not just patient behavior. But hey, let's blame the patients, as usual.
Johanna Pan
i use the hero device and it's been great. no more missin doses. the app tracks everything and even sends alerts. my mom takes 7 meds, so it's a lifesaver. but yeah, the pill organizers work well.
Elliot Alejo
Proper disposal is crucial. I always mix leftovers with coffee grounds and throw them in the trash. Pharmacies have take-back programs too-easy to use and safe. It's a simple step that makes a big difference.
Jenna Elliott
overprescribing is a problem but patients still misuse antibiotics. stopping early or sharing meds is dangerous. the data shows it. we need both better prescribing and better patient education.
lance black
Never share antibiotics. FDA ban. Done.
Pamela Power
It's astonishing how many people still don't understand the gravity of antibiotic misuse. The CDC's 2023 report clearly states that 34% of home antibiotic users are seniors, yet 38% of them don't complete courses. This isn't just negligence; it's a public health crisis. Improper disposal leads to 63% of U.S. waterways having antibiotic residues. The FDA's 2024 National Action Plan aims for a 15% reduction by 2027, but without stricter education, it's a pipe dream. I've seen firsthand how hospitals struggle with resistant bacteria. Every missed dose or leftover pill is a ticking time bomb for future generations. It's not enough to just know the guidelines-you must internalize them. Sharing antibiotics is reckless. Using old prescriptions without consulting a doctor is dangerous. Proper disposal isn't optional; it's mandatory. The science is clear: incomplete courses breed superbugs. The environmental impact is undeniable. We need systemic change, not just individual actions. But until then, each of us must take responsibility. It's not hard-set reminders, use apps, dispose correctly. Ignorance isn't an excuse. The stakes are too high. We can't afford to wait.



Write a comment