
For years, millions of people took a daily low-dose aspirin to prevent their first heart attack or stroke. It seemed simple: one pill, one less chance of something bad happening. But the science has changed - dramatically. Today, for most healthy adults, taking aspirin every day does more harm than good. The question isn’t whether aspirin works - it’s who should skip it entirely.
Why the Rules Changed
In the 1990s, studies like the Physicians’ Health Study showed that aspirin could lower heart attack risk. By the 2000s, doctors routinely recommended it for adults over 50. But those early studies didn’t fully account for the cost: bleeding. Not just minor nosebleeds or bruising - serious, life-threatening internal bleeding in the stomach or brain. By 2022, the U.S. Preventive Services Task Force (USPSTF) flipped its stance. Instead of recommending aspirin for people aged 50-59 with moderate heart disease risk, they now say: don’t start it if you’re 60 or older. For those between 40 and 59, it’s not a blanket yes - it’s a personal decision, only if you’re at high heart risk and low bleeding risk. The American Heart Association and American College of Cardiology followed suit. Their 2019 guidelines already said aspirin shouldn’t be used routinely for primary prevention. Now, even the most cautious experts agree: the benefits are too small, and the risks are too real.Who Definitely Should Skip Aspirin
If you’re 60 or older and don’t have heart disease, you should not start daily aspirin. Period. The data is clear: for every 1,000 people over 60 taking aspirin for 10 years, about 1.6 will have a major bleed - like a stomach ulcer that won’t stop bleeding or a brain hemorrhage. Meanwhile, only about 0.9 will avoid a heart attack. That’s not a win. It’s a loss. Even if you’re younger, skip aspirin if you have any of these:- A history of stomach ulcers or bleeding in the digestive tract
- Regular use of NSAIDs like ibuprofen or naproxen
- Taking blood thinners like warfarin, apixaban, or rivaroxaban
- Uncontrolled high blood pressure
- Kidney disease or liver disease
- A history of bleeding in the brain
- Being over 70 - even if you feel fine
Who Might Still Benefit - But Only After a Deep Dive
There’s a small group where aspirin might still make sense. But it’s not about age alone. It’s about precision. You might consider aspirin if you’re 40-59, have a 10-year cardiovascular disease risk of 10% or higher (calculated using the Pooled Cohort Equations), and have no bleeding risk factors. Even then, it’s not automatic. You need to talk through it with your doctor. Some people in this group have hidden risk markers that change the equation:- Coronary artery calcium (CAC) score over 100 - meaning visible plaque in heart arteries
- Lipoprotein(a) levels above 50 mg/dL - a genetic risk factor for clotting
- Diabetes with additional risk factors like high blood pressure or smoking
The Cost of Being Wrong
Many people who take aspirin daily don’t realize they’re not in the group that benefits. A 2023 Mayo Clinic survey found 41% of adults 60+ still take aspirin for prevention - even after new guidelines came out. Why? Fear. “I was told to take it for 20 years,” one 68-year-old woman told her doctor. “I’m scared if I stop, I’ll have a heart attack.” But stopping aspirin doesn’t cause a rebound heart attack. That’s a myth. The risk comes from continuing it when you shouldn’t. Major bleeding events cost Medicare an average of $1,200 per case. And those aren’t just financial costs - they’re hospitalizations, long recovery times, and sometimes death. Worse, doctors are still giving mixed messages. A 2023 study in JAMA Internal Medicine found 57% of patients reported getting conflicting advice. Cardiologists are more likely to keep prescribing aspirin than primary care doctors. One reason? Cardiologists see patients who’ve already had heart problems - so they’re used to treating secondary prevention. Primary prevention is different. You’re healthy. You’re not supposed to be bleeding to stay healthy.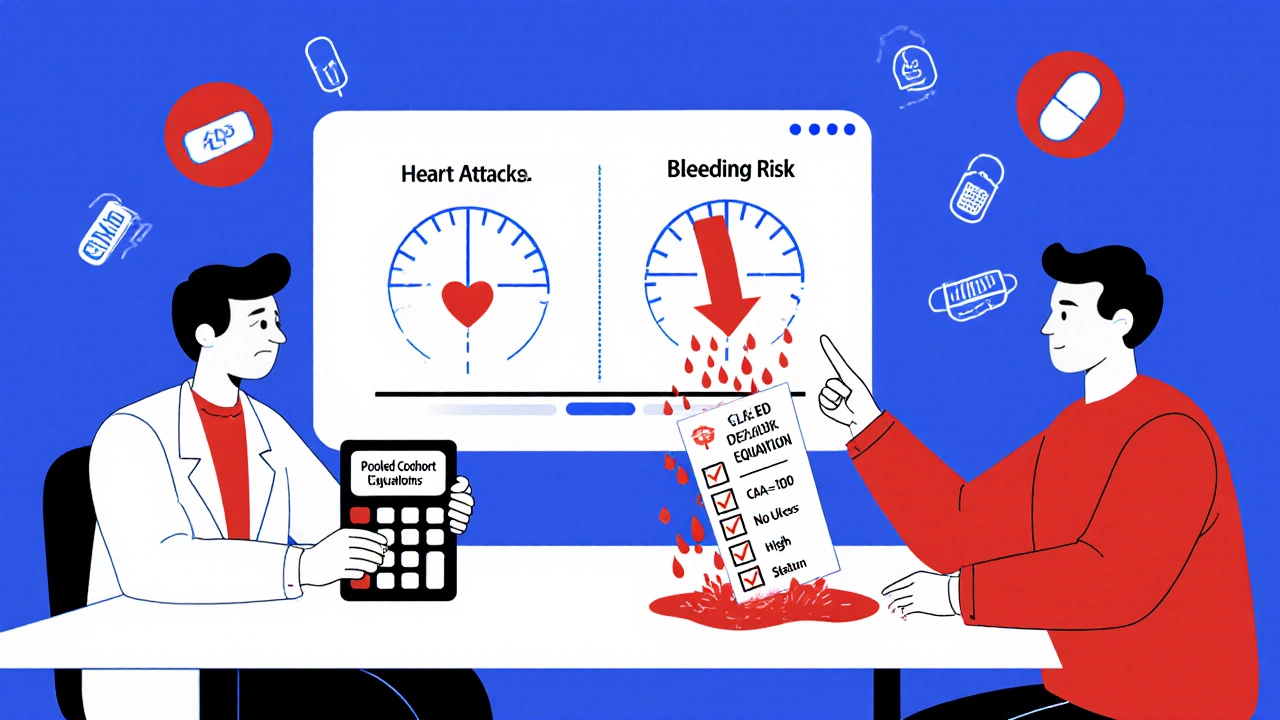
What to Do Instead
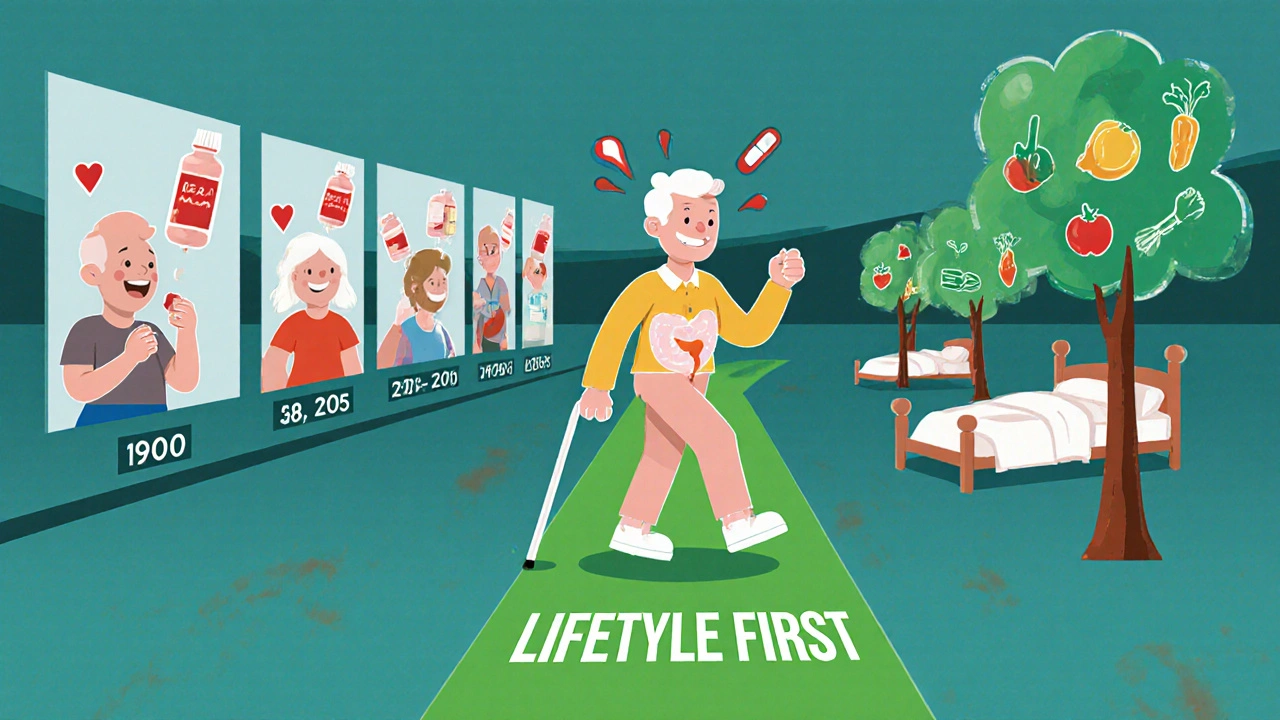
If you’re not taking aspirin for primary prevention, what should you do? Focus on what actually moves the needle:- Manage blood pressure - aim for under 120/80
- Keep cholesterol in check - especially LDL
- Don’t smoke - ever
- Get 150 minutes of moderate exercise a week
- Eat more vegetables, beans, whole grains, and fish
- Control your weight - even a 5% loss helps
- Check your blood sugar - especially if you’re over 45
What About Diabetes?
People with diabetes are often told to take aspirin. But the 2025 AHA/ACC guidelines updated this too. Now, aspirin may be considered only for diabetics aged 40-70 with a 10-year ASCVD risk of 15% or higher - and no bleeding risk. That means most diabetics under 40, or over 70, should skip it. Even if you have diabetes, if your arteries are clean and your blood pressure is good, aspirin won’t help. And it might hurt.Tools to Help You Decide
You don’t need to guess. Use these free tools:- ACC/AHA Pooled Cohort Equations - calculates your 10-year heart disease risk
- HAS-BLED score - checks your bleeding risk (factors: high blood pressure, liver/kidney disease, stroke history, lab values, drugs, age, bleeding history)
- AHA’s ‘Know Your Risk’ calculator - simple, patient-friendly version
What If You’re Already Taking It?
If you’ve been on daily aspirin for years and you’re over 60, talk to your doctor about stopping. Don’t quit cold turkey - but don’t keep taking it just because “it’s always been part of my routine.” A 2023 study found that patients who stopped aspirin after the 2022 guidelines had no increase in heart events - and fewer stomach problems. One Reddit user wrote: “At 62, my doctor took me off aspirin after the USPSTF update. I’ve had zero issues since.” If you’re under 60 and have high risk markers - like a CAC score of 350 - your doctor might still recommend it. But that’s a personalized call, not a default.The Bottom Line
Aspirin isn’t a magic bullet. It’s a tool with sharp edges. For most healthy people, especially those over 60, the edges cut deeper than the benefits. The era of “take one a day” for prevention is over. If you’re healthy, active, and don’t have heart disease, you don’t need aspirin. You need better sleep, better food, more movement, and a clear conversation with your doctor - not a pill.Frequently Asked Questions
Is it safe to stop taking aspirin if I’ve been on it for years?
Yes. Stopping aspirin doesn’t cause a rebound effect or sudden increase in heart attacks. The risk comes from continuing it when you shouldn’t. If you’re over 60 and taking it for primary prevention, talk to your doctor about stopping. Most people experience fewer stomach issues and no increase in heart events after discontinuing.
Can I take aspirin if I have high blood pressure?
Not unless your blood pressure is well-controlled. Uncontrolled high blood pressure increases the risk of brain bleeding. Aspirin thins the blood, which makes bleeding more likely. If your blood pressure is above 140/90, aspirin is not recommended for primary prevention.
Does aspirin help prevent stroke in healthy people?
For most healthy people, no. Aspirin slightly reduces the risk of ischemic stroke (caused by clots), but increases the risk of hemorrhagic stroke (caused by bleeding in the brain). In people over 60, the bleeding risk outweighs any small benefit. The net effect is zero or negative.
What’s the difference between primary and secondary prevention?
Primary prevention means taking aspirin to prevent a first heart attack or stroke in someone with no history of heart disease. Secondary prevention means taking it after you’ve already had a heart attack, stroke, or stent. For secondary prevention, aspirin is still strongly recommended. The guidelines only changed for people who’ve never had a cardiovascular event.
Are there alternatives to aspirin for heart health?
Yes - and they’re more effective. Focus on lifestyle: regular exercise, a plant-rich diet, quitting smoking, managing blood pressure and cholesterol. Statins are often a better choice than aspirin for people with high cholesterol or diabetes. For those with very high risk, doctors may recommend newer medications like PCSK9 inhibitors. Aspirin isn’t the only tool - and it’s rarely the best one for prevention.
Why do some doctors still recommend aspirin?
Some doctors rely on old habits or see patients who’ve had heart events and assume the same advice applies. Others may not be up to date on the latest guidelines. Patient pressure also plays a role - many people believe aspirin is protective and don’t want to stop. But the evidence is clear: for primary prevention, the risks now outweigh the benefits for most.
Can I take aspirin occasionally for pain instead of daily?
Yes. Taking aspirin occasionally for headaches, muscle pain, or fever doesn’t carry the same bleeding risk as daily use. The danger comes from long-term, daily exposure. If you only take it when needed, you’re not increasing your risk of major bleeding.
swatantra kumar
Bro this is why I stopped taking aspirin last year 😌 No more stomach issues, no more 'is this bleeding?' paranoia. Just chillin' with my green tea and yoga. Life's better when you stop listening to doctors who still think the 90s never ended 🙌
robert cardy solano
I was on it for 15 years after my dad had a heart attack. Turns out he was in the 1% who actually benefited. I'm 61, healthy, no risk factors. Doctor finally said 'stop.' Been off for 8 months. Zero problems. Funny how we cling to pills like they're talismans.
Lemmy Coco
i just found out my doc gave me aspirin b/c he was 'too busy' to run the pooled cohort calc. i asked for the numbers and he said 'you're over 60 so probably not.' i'm not mad just disappointed. why not just use the free tools? its not hard.
serge jane
The real tragedy isn't that people are taking aspirin it's that we've outsourced our health to a pill culture. We want a magic bullet because we don't want to change our diet or move more or sleep better or manage stress. Aspirin was never the answer it was the distraction. The fact that the guidelines changed doesn't surprise me what surprises me is that it took this long for anyone to notice that prevention isn't pharmaceutical it's behavioral. We treat symptoms not causes and then wonder why we're all broken.
Cinkoon Marketing
I mean I get it but like... what if you're just... cautious? I'm 52, borderline prediabetic, mom had a stroke at 68, and I'm scared. I don't want to be the one who 'didn't do enough.' I know the stats but fear doesn't care about stats. And honestly? My doctor still says 'it's fine.' So I keep taking it. Not because I believe it works but because I don't want to regret not trying.
rob lafata
Let me guess - you're one of those people who thinks 'natural' means 'safe.' Wake up. Aspirin is a drug. A powerful one. And if you're not actively managing your bleeding risk you're playing Russian roulette with your GI tract. Meanwhile you're eating gluten-free donuts and calling it 'wellness.' The real problem isn't aspirin it's the delusional health influencers who tell you you don't need doctors. You need a blood test. Not a juice cleanse.
Pawan Jamwal
This is why America is weak. In India we don't waste time with 'guidelines' we just take aspirin and pray. If you bleed you were weak anyway. This over-analysis is why your life expectancy is dropping. Take the pill. Be strong. Don't let some USPSTF paper make you soft.
Bill Camp
THEY KNOW. THEY ALL KNOW. This is part of the pharmaceutical agenda to push statins and expensive monoclonal antibodies. Aspirin costs 5 cents. Statins cost $200 a month. Who profits? Big Pharma. Who gets hurt? You. The real enemy isn't aspirin it's the system that wants you dependent on expensive drugs while telling you to 'take one pill a day' like a good little consumer. Wake up. This is control.
Matthew McCraney
I stopped taking it after reading this and now my blood pressure is higher and I'm paranoid every time I get a headache. I think they're lying about the bleeding risk. I read somewhere that the government hides the truth about aspirin because it's cheap. I'm not taking any more meds. I'm going to eat raw garlic and drink apple cider vinegar. My neighbor's dog died from a heart attack last week. Coincidence? I think not.





Write a comment