When your liver starts acting up, it’s easy to assume it’s just one problem-maybe fatty liver, maybe hepatitis. But sometimes, the signs don’t fit neatly into one box. You might have high alkaline phosphatase like someone with PBC, but also elevated ALT and ANA like someone with AIH. That’s not a mistake. It’s an overlap syndrome.
What Exactly Is an Autoimmune Liver Overlap?
Autoimmune overlap syndromes happen when a person shows clear signs of two or more autoimmune liver diseases at the same time. The most common mix is AIH-PBC-Autoimmune Hepatitis and Primary Biliary Cholangitis. Less common, but still documented, are cases with features of PSC (Primary Sclerosing Cholangitis) thrown in. These aren’t rare flukes. Studies show up to 7% of people diagnosed with AIH also meet criteria for PBC, and 2-19% of PBC patients show AIH-like features.
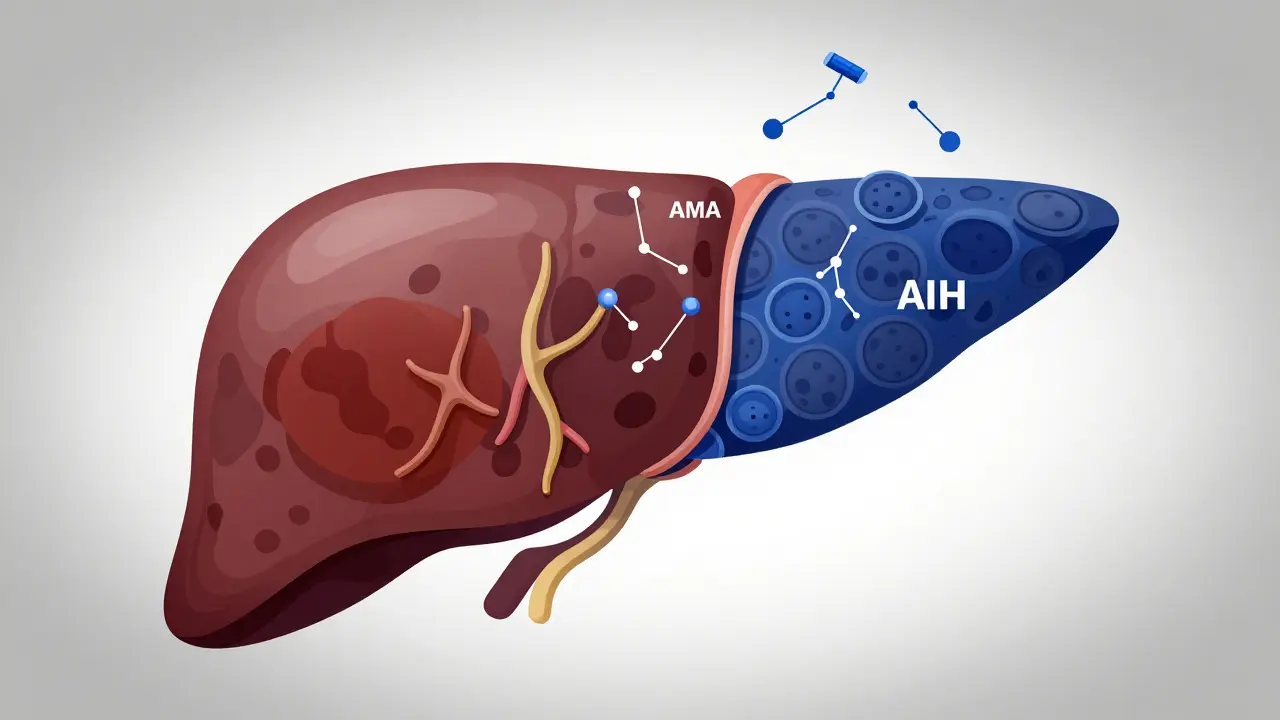
It’s not just about numbers. It’s about what’s happening inside the liver. In pure PBC, the immune system attacks the small bile ducts. In AIH, it targets the liver cells themselves. When both happen together, the damage gets messy. The liver doesn’t just get clogged-it gets inflamed, scarred, and stressed from multiple angles.
How Do You Tell Them Apart?
Each disease has its fingerprint:
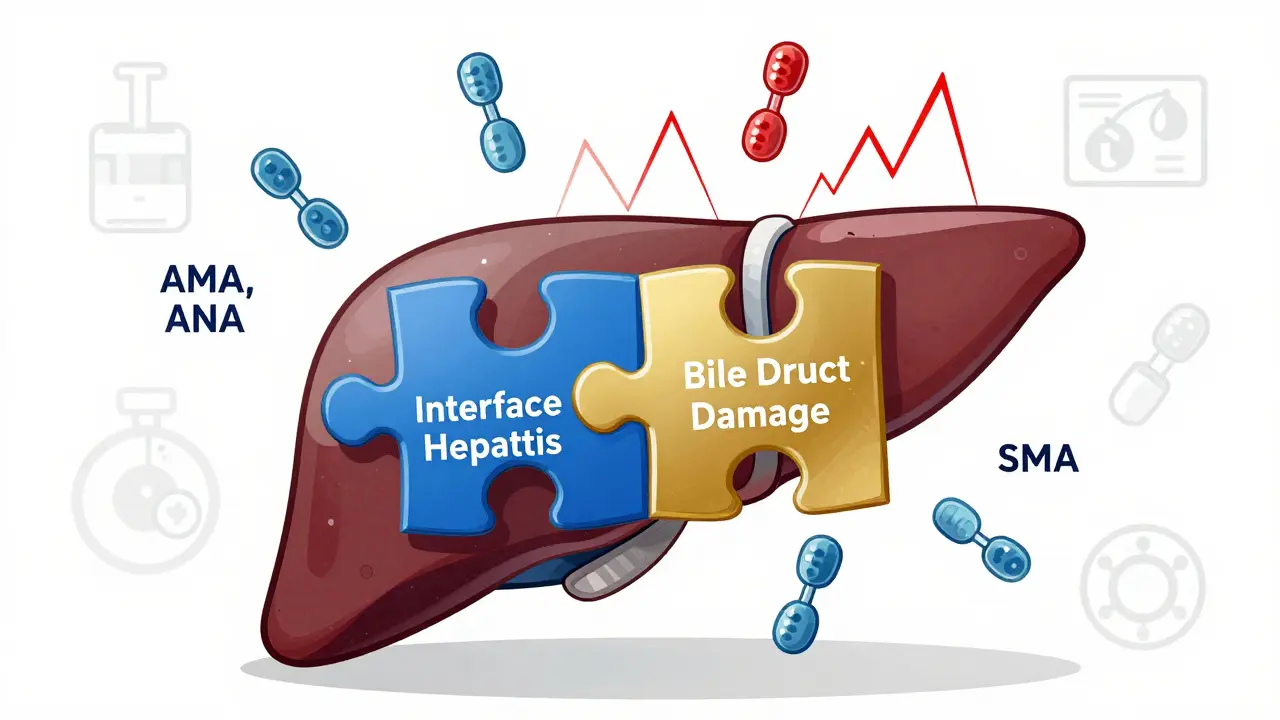
- PBC: High ALP and GGT (cholestatic pattern), positive AMA (anti-mitochondrial antibodies) in 90-95% of cases, elevated IgM, and bile duct damage seen on biopsy.
- AIH: High ALT and AST (hepatocellular pattern), elevated IgG, positive ANA or SMA (smooth muscle antibodies), and interface hepatitis on biopsy.
- PSC: Also cholestatic, but AMA is negative. Often linked to IBD (inflammatory bowel disease), with a “beaded” bile duct appearance on MRCP or ERCP.
But in overlap cases, these lines blur. A patient might have AMA-positive PBC and elevated IgG and interface hepatitis-two hallmarks of AIH. That’s not a misdiagnosis. That’s an overlap.
The tricky part? There’s no single test that confirms it. Diagnosis relies on combining blood work, antibody profiles, and liver biopsy results. The most widely used criteria require meeting at least two of the three diagnostic points for both diseases. For example: ALP >2x upper limit + AMA positive (for PBC) and IgG >2x upper limit + interface hepatitis (for AIH).
Is PBC and PSC Overlap Real?
Here’s where things get controversial. You’ll read case reports of patients with features of both PBC and PSC-AMA positive, bile duct strictures, elevated ALP. But major liver societies, including the European Association for the Study of the Liver, say there’s no clear evidence these are true overlaps.
Why? Because PSC and PBC are fundamentally different in how they develop. PSC is tied to immune dysregulation in the gut (often with ulcerative colitis), while PBC is linked to molecular mimicry and bile duct-specific autoimmunity. The bile duct damage in PSC looks like scarring and narrowing; in PBC, it’s more like a slow, targeted destruction of small ducts. When both show up, experts often suspect one of two things: either the patient has PSC with a coincidental AMA positivity (which happens in 5-10% of PSC cases), or they’re misclassified.
Bottom line: AIH-PBC overlap is real and recognized. PBC-PSC overlap? Still a mystery. Most hepatologists treat it as a variant of PSC, not a true overlap.
Treatment Isn’t One-Size-Fits-All
Standard treatment for PBC is ursodeoxycholic acid (UDCA). For AIH, it’s prednisone and azathioprine. But if you have both? UDCA alone often isn’t enough.
Studies show 30-40% of AIH-PBC overlap patients don’t respond well to UDCA alone. Their transaminases stay high. Their inflammation doesn’t calm down. That’s when immunosuppressants get added. A 2020 case report followed a 39-year-old man who was on UDCA for years-his ALP improved, but his ALT stayed stubbornly high. Only after adding azathioprine did his liver enzymes normalize.
It’s not just about drugs. It’s about timing. Starting immunosuppression too late means more scarring. Waiting too long can lead to cirrhosis. About 30-40% of untreated overlap patients develop cirrhosis within 10 years-similar to pure disease, but with more unpredictable progression.
Doctors now treat overlap cases based on what’s dominant. If AIH features are stronger, start with steroids. If PBC is clearer, begin with UDCA and add immunosuppression if liver enzymes don’t improve in 6 months. There’s no official guideline, but the consensus is: monitor closely, adjust early, and don’t wait for full cirrhosis to act.
Why Misdiagnosis Is Common
Most general practitioners and even some gastroenterologists have never seen an overlap case. They see high ALP and think “PBC.” They see high ALT and think “AIH.” They don’t look for both.
Here’s what often gets missed:
- AMA-negative PBC patients with sp100 or gp210 antibodies-these are easy to overlook if you’re not testing for them.
- ANA positivity in PBC patients-common (up to 50%), but often dismissed as “just a false positive.”
- Patients with mild symptoms: fatigue, joint pain, itching. These are vague. They get labeled as stress or aging.
Studies estimate misdiagnosis rates in community practice at 15-20%. That’s one in five people being treated for the wrong thing-or only half the problem.
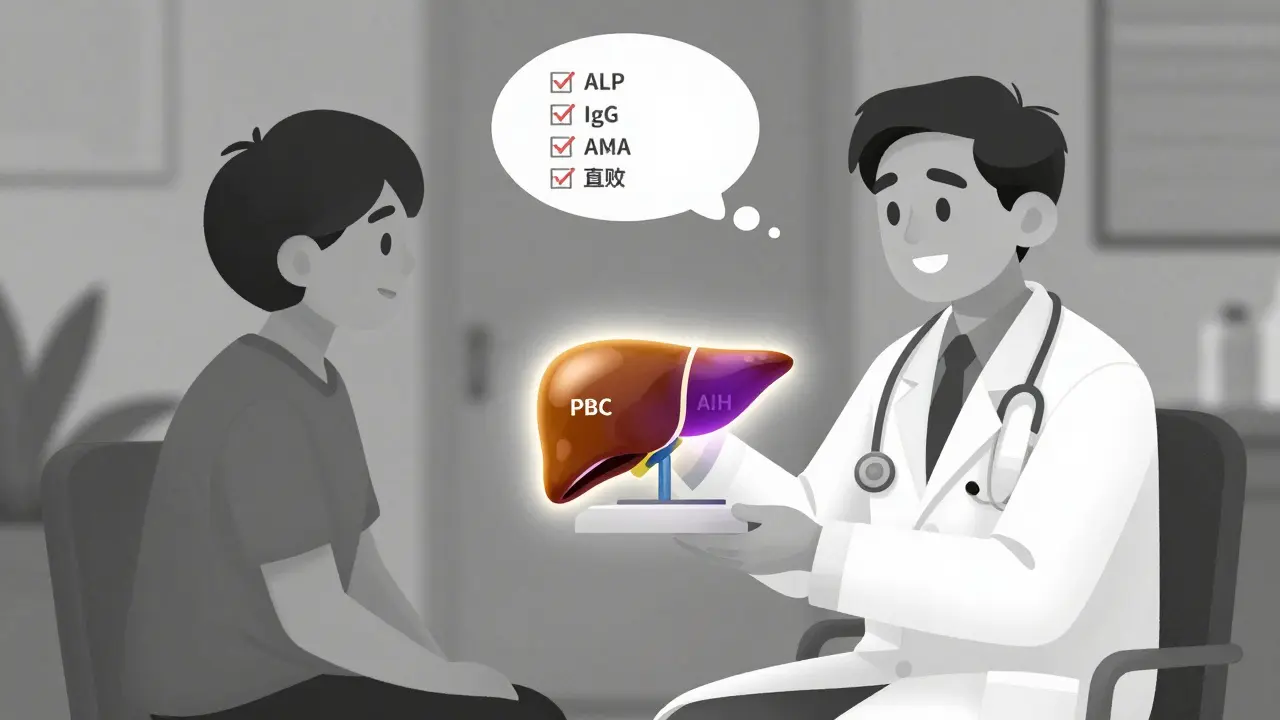
The fix? Always test for both AMA and ANA/SMA in anyone with unexplained liver enzyme abnormalities. If ALP is high, check IgG. If IgG is high, check AMA. Don’t stop at the first positive result.
What Happens After Diagnosis?
Once you’ve got the diagnosis, it’s not a one-and-done situation. These patients need lifelong monitoring.
They need:
- Every 6 months: liver enzymes, IgG, IgM, and autoantibodies.
- Annual imaging: ultrasound or FibroScan to track fibrosis.
- Regular screening for complications: osteoporosis (common in PBC), colon cancer (if PSC is suspected), and hepatocellular carcinoma (if cirrhosis develops).
Transplantation is still the last resort-but even then, outcomes differ. AIH-PBC patients who get transplants tend to have lower recurrence rates than those with pure AIH. But if PSC features are present, recurrence in the new liver is more likely.
The Bigger Picture: A Spectrum, Not Separate Diseases
The field is shifting. Experts like Dr. Pietro Invernizzi and Dr. Marlyn Mayo argue that autoimmune liver diseases aren’t separate boxes-they’re points on a spectrum. Some people have pure AIH. Others have pure PBC. Others fall in between, with mixed features.
That’s why overlap syndromes aren’t anomalies. They’re clues. They tell us the immune system doesn’t always follow our tidy categories. It’s messy. It’s complex. And it’s changing how we think about liver autoimmunity.
Future research is focused on validating diagnostic criteria and identifying new autoantibodies. By 2025, we may have clearer guidelines. Until then, the best approach is simple: think beyond the single diagnosis. If the picture doesn’t fit, look for the pieces you missed.
Frequently Asked Questions
Can you have PBC and AIH at the same time?
Yes. AIH-PBC overlap is the most common autoimmune liver overlap syndrome. It’s diagnosed when a patient meets key criteria for both diseases-like positive AMA and elevated IgG with interface hepatitis on biopsy. It’s not rare-studies show it affects up to 7% of AIH patients and 2-19% of PBC patients.
Is PBC-PSC overlap a real condition?
No, not according to current expert consensus. While there are case reports of patients with features of both, major liver associations like EASL and AASLD state there’s no clear evidence that PBC and PSC truly overlap. AMA positivity can occur in PSC (5-10% of cases), but that doesn’t mean it’s a true overlap. Most experts believe these are either misclassified PSC cases or coincidental findings.
What’s the treatment for AIH-PBC overlap?
It’s combination therapy. Ursodeoxycholic acid (UDCA) is started for the PBC component, but if liver enzymes (ALT/AST) stay high after 6 months, immunosuppressants like prednisone or azathioprine are added. About 30-40% of patients need both to control inflammation and prevent scarring. UDCA alone usually isn’t enough.
How do doctors diagnose an overlap syndrome?
They combine blood tests, antibodies, and liver biopsy. For AIH-PBC, they look for: (1) elevated ALP and positive AMA (for PBC), and (2) elevated IgG and interface hepatitis on biopsy (for AIH). You need features from both diseases to confirm it. No single test does it alone.
Can overlap syndromes be cured?
No cure exists yet. But with early, correct treatment, progression to cirrhosis can be slowed or stopped in many cases. Lifelong monitoring is required. Some patients stabilize for decades on combination therapy. The goal isn’t cure-it’s control and prevention of complications like liver failure or cancer.
What to Do Next
If you’ve been diagnosed with PBC, AIH, or PSC-and your symptoms don’t fully match, or your treatment isn’t working-it’s worth asking for a second look. Request a full autoimmune panel: AMA, ANA, SMA, IgG, IgM. Ask if a liver biopsy has been done. If not, and your enzymes are still abnormal, ask why.
Overlap syndromes are rare, but they’re real. And they need more than a quick diagnosis. They need careful, ongoing care. Don’t settle for the first answer. Push for the full picture. Your liver depends on it.
Kelly McRainey Moore
This was so clear and helpful-thanks for laying it out like this. I’ve been chasing answers for my mom’s liver numbers for months, and this finally made sense.
lokesh prasanth
AMA+ and IgG high? That’s not overlap. That’s bad testing.
Rod Wheatley
So many people get dismissed because doctors don’t look beyond the first positive. This post is a lifeline. If you’re tired of being told ‘it’s just stress’-keep pushing. You’re not crazy. There’s a reason your enzymes won’t normalize.
Jarrod Flesch
Been living with AIH-PBC for 8 years. UDCA + azathioprine saved me. Still tired. Still itchy. But no cirrhosis. 🙌
PS: Don’t skip the FibroScan. It’s not scary. I cried the first time I saw my liver looked ‘okay.’
Andrew Rinaldi
The idea that autoimmune diseases exist on a spectrum rather than in boxes feels deeply true. Our bodies don’t read textbooks. They just react. Maybe the real mistake isn’t the overlap-it’s our need to categorize everything neatly.
Gerard Jordan
Just shared this with my cousin who’s been told ‘it’s probably fatty liver’ for 3 years. She’s finally getting the full panel done next week. 🤞
Thank you for writing this. So many people need to see this.
Samuel Mendoza
PBC-PSC overlap is fake. Stop making up diseases.
Glenda Marínez Granados
So we’re supposed to believe the immune system is just… confused? Like it forgot its flashcards and picked two diseases at once? 😏
Coral Bosley
I’ve been screaming into the void for years about how doctors ignore the IgG. Now I feel seen. I cried reading this. Not because I’m sad-because someone finally said it out loud.
MAHENDRA MEGHWAL
Respectfully, the diagnostic criteria outlined herein are in accordance with the latest EASL guidelines, and the clinical implications are both significant and underappreciated in primary care settings.
Dee Monroe
You know what’s beautiful about this? It’s not just about liver enzymes or antibodies-it’s about how we treat people who don’t fit the mold. So many of us have been told we’re ‘too complicated’ or ‘not a good candidate’-but what if we’re not complicated? What if the system is just too lazy to look deeper? This post isn’t just medical advice-it’s a quiet rebellion against the idea that one diagnosis is enough. Keep pushing for the full picture. Your body deserves nothing less.
Ben McKibbin
The misdiagnosis rate of 15-20%? That’s criminal. We’re not talking about a cold-we’re talking about slow, silent organ destruction. If your doctor won’t test for AMA AND ANA together, find a new one. Period.
Barbara Mahone
Interesting how the immune system blurs lines-makes you wonder if all autoimmune conditions are just variations of the same underlying misfire. Maybe the real disease isn’t PBC or AIH… it’s the immune system’s inability to read its own manual.
michelle Brownsea
Let’s be real: the medical establishment still treats autoimmune diseases like they’re separate Lego sets. But the body doesn’t build itself in neat little boxes. When you have AMA AND interface hepatitis? That’s not an ‘overlap’-it’s the immune system screaming that your body’s borders are collapsing. And yes, it’s terrifying. But it’s also a clue. A clue that we’ve been looking at autoimmunity through a cracked lens. Stop calling it ‘rare.’ It’s just underdiagnosed because we’re too comfortable with labels. We need to stop treating symptoms and start listening to the whole damn system.
Melanie Pearson
As a former hospital administrator, I can confirm: most clinics don’t have the budget to run full autoimmune panels. This is a systemic failure, not a diagnostic oversight. Until we fund proper liver care, patients will keep falling through the cracks.




Write a comment