Angina Treatment Option Selector
Patient Assessment
Treatment Insights
Ranolazine offers a unique mechanism targeting late sodium current without significantly affecting heart rate or blood pressure. It's particularly valuable for patients who cannot tolerate beta-blockers or calcium channel blockers, or when additional therapy is needed.
Treatment Recommendations
Ranolazine (Ranolazine)
Recommended for patients with moderate angina who need an alternative to beta-blockers or calcium channel blockers.
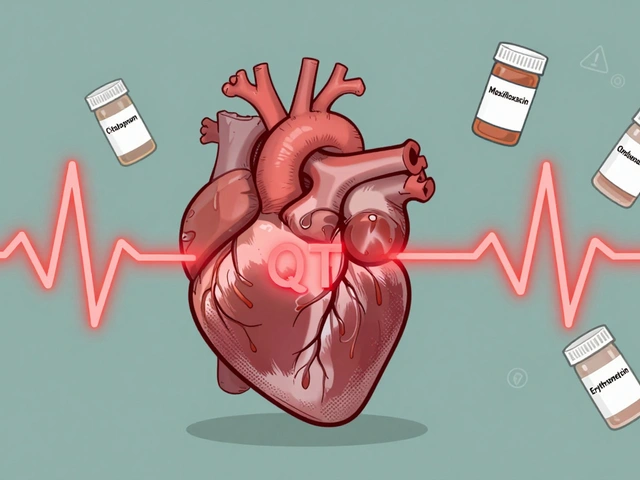
Minimal impact on heart rate and blood pressure. Consider monitoring QT interval if other CYP3A4 inhibitors are used.
Beta-blockers (e.g., Metoprolol)
Not recommended for patients with asthma or severe bradycardia.
May cause bradycardia and reduce exercise tolerance.
Calcium Channel Blockers (e.g., Amlodipine)
Not recommended for patients with heart failure or severe hypotension.
May cause peripheral edema and reflex tachycardia.
Nitrates (e.g., Nitroglycerin)
Ideal for acute symptom relief but limited for chronic management.
Useful for breakthrough chest pain but develops tolerance with continuous use.
Key Takeaways
- Ranolazine works by reducing the late sodium current in heart cells, a mechanism different from traditional beta‑blockers or nitrates.
- Compared with beta‑blockers, calcium‑channel blockers, nitrates and newer agents like ivabradine, Ranolazine has a lower impact on heart rate and blood pressure.
- Typical side‑effects of Ranolazine are constipation, dizziness and mild nausea; serious concerns include QT‑interval prolongation.
- Cost varies widely - generic ranolazine can cost about $120 for a 30‑day supply in the US, while older drugs such as nitroglycerin are often cheaper.
- Best suited for patients who cannot tolerate beta‑blockers or calcium‑channel blockers, or who need an additional drug to control angina despite optimal therapy.
What is Ranolazine?
When treating chronic stable angina, Ranolazine is an anti‑anginal medication that targets the late inward sodium current in cardiac myocytes, improving myocardial oxygen efficiency without changing heart rate or blood pressure. The brand name Ranolazine (sold as Ranexa in the United States) received FDA approval in 2006 and has since been incorporated into many treatment guidelines.
Ranolazine is taken orally, usually in doses of 500mg twice daily, titrated up to 1000mg twice daily based on tolerance. Its half‑life averages 7hours, allowing flexible dosing schedules.
Why Compare Ranolazine with Alternatives?
Patients with chronic stable angina often need more than one medication to achieve symptom relief. Traditional options-beta‑blockers, calcium‑channel blockers, long‑acting nitrates-work through heart‑rate reduction, vasodilation, or preload reduction. Ranolazine offers a distinct pathway, which can be a game‑changer for those who have contraindications or adverse reactions to the classics.
Below we line up the most widely used alternatives and highlight where Ranolazine stands on key dimensions.
Alternative Anti‑Anginal Drugs
Metoprolol is a selective beta‑1 blocker that lowers heart rate and myocardial oxygen demand, typically prescribed at 50-200mg daily.
Amlodipine is a dihydropyridine calcium‑channel blocker that relaxes arterial smooth muscle, reducing afterload, usually 5-10mg once daily.
Ivabradine selectively inhibits the funny (If) current in the sino‑atrial node, decreasing heart rate without affecting contractility, taken at 5mg twice daily.
Nicorandil combines nitrate‑like vasodilation with potassium‑channel activation, improving coronary blood flow, dosed 5-20mg three times daily.
Nitroglycerin is a short‑acting nitrate that dilates veins and arteries, commonly used as a sublingual tablet for acute attacks, 0.3-0.6mg as needed.

Side‑Effect Profiles
Understanding tolerability is crucial because many patients stop therapy due to adverse events.
- Ranolazine: constipation (≈10%), dizziness, nausea; rare but serious QT‑prolongation, especially when combined with CYP3A4 inhibitors.
- Metoprolol: fatigue, bradycardia, bronchospasm in asthmatics, sexual dysfunction.
- Amlodipine: peripheral edema, gingival hyperplasia, reflex tachycardia.
- Ivabradine: luminous visual phenomena (phosphenes), bradycardia.
- Nicorandil: headache, flushing, rare ulceration of the gastrointestinal tract.
- Nitroglycerin: headache, hypotension, tolerance with continuous use.
Drug Interactions and Contraindications
Ranolazine is metabolised by CYP3A4 and CYP2D6, so co‑administration with strong inhibitors (e.g., ketoconazole, clarithromycin) can raise plasma levels and increase QT risk. It is contraindicated in patients with pre‑existing QT>500ms.
Metoprolol should be avoided in severe asthma or second‑/third‑degree AV block. Amlodipine requires caution in severe hepatic impairment. Ivabradine is contraindicated in acute decompensated heart failure and in patients with a resting heart rate <70bpm.
Nicorandil should not be used in patients with severe hypotension or active peptic ulcer disease. Nitroglycerin interacts with phosphodiesterase‑5 inhibitors, causing dangerous hypotension.
Cost Comparison (US 2025)
| Drug | Mechanism | Typical Dose | Half‑Life | Common Side‑Effects | Approx. 30‑Day Cost (USD) |
|---|---|---|---|---|---|
| Ranolazine (Ranexa) | Late Na⁺ current inhibition | 500‑1000mg BID | ≈7h | Constipation, dizziness, nausea | $120 (generic) |
| Metoprolol | β₁‑blockade | 50‑200mg QD | ≈3‑7h | Fatigue, bradycardia, bronchospasm | $8 (generic) |
| Amlodipine | Dihydropyridine Ca²⁺‑channel block | 5‑10mg QD | ≈30‑50h | Edema, flushing, gingival growth | $12 (generic) |
| Ivabradine | If‑current inhibition | 5mg BID | ≈2h | Phosphenes, bradycardia | $75 (generic) |
| Nicorandil | Nitrate + K⁺‑channel opener | 5‑20mg TID | ≈1‑2h | Headache, GI ulceration | $30 (generic) |
| Nitroglycerin (SL) | NO donor - venous & arterial dilation | 0.3‑0.6mg as needed | ≈1‑3min (onset) | Headache, hypotension | $5 (over‑the‑counter) |
When to Choose Ranolazine
If a patient is already on a maximally tolerated beta‑blocker or calcium‑channel blocker and still experiences angina, adding Ranolazine can provide incremental relief without further lowering blood pressure or heart rate. It also shines for patients with asthma (who can’t handle β‑blockers) or for those with peripheral edema from amlodipine.
Because Ranolazine does not cause reflex tachycardia, it can be paired safely with nitrates, offering a multi‑modal approach: nitrates for acute episodes, Ranolazine for chronic symptom control.

When Alternatives Might Be Better
- Metoprolol remains first‑line for patients with hypertension and a need to blunt sympathetic tone.
- Amlodipine is preferred when blood pressure control is a primary goal, especially in elderly patients with isolated systolic hypertension.
- Ivabradine fits patients with resting heart rates >70bpm who cannot tolerate β‑blockers yet need rate control.
- Nicorandil is useful for patients with both coronary spasm and microvascular disease, thanks to its dual mechanism.
- Nitroglycerin is unbeatable for rapid relief of breakthrough chest pain.
Practical Decision Checklist
- Assess current anti‑anginal regimen and residual symptom burden.
- Identify contraindications (e.g., asthma, severe hypotension, QT prolongation).
- Check for drug‑drug interactions-especially CYP3A4 inhibitors with Ranolazine.
- Consider patient preference regarding dosing frequency and side‑effect tolerance.
- Review cost and insurance coverage; generic Ranolazine may be affordable, but some plans still favor older generics.
- Start low (500mg BID) and titrate based on symptoms and ECG monitoring.
Monitoring and Follow‑Up
Baseline ECG is essential before starting Ranolazine to document QT interval. After titration, repeat ECG within 2weeks. If QT>500ms, reduce dose or discontinue.
For all anti‑anginals, evaluate symptom diaries, exercise tolerance, and any new adverse effects at each visit. Adjust therapy based on a shared decision‑making model.
Frequently Asked Questions
Can Ranolazine be used alone for chronic angina?
Guidelines recommend Ranolazine as add‑on therapy when a beta‑blocker or calcium‑channel blocker alone does not control symptoms. Monotherapy is occasionally used in patients who cannot tolerate other classes, but evidence supports combination use for maximum benefit.
Does Ranolazine affect blood pressure?
Ranolazine has minimal impact on systemic blood pressure, which is why it is attractive for patients already on antihypertensive regimens.
What should I do if I develop constipation on Ranolazine?
Increase dietary fiber, hydrate well, and consider a mild stool softener. If constipation persists, discuss dose reduction or switching with your physician.
Is Ranolazine safe with statins?
Yes, most statins are safe. However, simvastatin metabolism overlaps with CYP3A4, so dose adjustments may be needed. Always inform your clinician about all concurrent meds.
How quickly does Ranolazine start working?
Patients often notice improvement within 1‑2 weeks, but full effect may take up to 4 weeks of consistent dosing.
Bottom Line
Ranolazine offers a unique mechanism that fills the gap when classic heart‑rate‑lowering drugs aren’t enough or aren’t tolerated. Its side‑effect profile is generally mild, but the QT‑prolongation risk demands careful ECG monitoring. Cost is higher than cheap generics like metoprolol, yet still reasonable for a newer agent. By weighing symptom control, comorbidities, drug interactions, and price, clinicians can decide whether Ranolazine or one of its alternatives is the right fit for each patient.
Moumita Bhaumik
Don’t be fooled by pharma; they’re pushing Ranolazine to keep us dependent.
Sheila Hood
Alright, let’s break down the basics. Ranolazine does a neat job of targeting the late sodium current without the classic heart‑rate knock‑down you see with beta‑blockers. The trade‑off is its QT‑prolongation potential, especially with CYP3A4 inhibitors – something the pamphlet barely mentions. Cost-wise, $120 a month isn’t cheap, but it beats the nightly nitrate titration for many patients. You still need a baseline ECG and a follow‑up in two weeks, which adds clinic time. Compared to nitrates, you avoid tolerance, but you gain a monitoring burden. If a patient can tolerate a beta‑blocker, that stays first‑line in my view. Still, for those who can’t, Ranolazine is a solid add‑on.
Melissa Jansson
While the mainstream narrative glorifies Ranolazine as a silver bullet for refractory angina, the pharmacologic realities are far more nuanced. First, the drug's mechanism- inhibition of the late inward Na+ current- is a double‑edged sword; it improves myocardial efficiency but also predisposes to electrophysiologic instability when co‑administered with CYP3A4 inhibitors such as clarithromycin. Second, the QT‑prolongation risk, often dismissed as a peripheral concern, can precipitate torsades in a subset of patients with subclinical repolarization abnormalities. Third, the comparative pharmacoeconomics are deceptive: while the headline $120/month seems modest, it fails to account for the downstream costs of ECG monitoring, potential dose adjustments, and the hidden expenses of adverse event management. Fourth, the meta‑analyses that underwrite the guideline endorsements suffer from heterogeneous study populations, making extrapolation to real‑world practice precarious. Fifth, the tolerability profile- constipation, dizziness, and nausea- may be deemed mild, yet in a chronic disease setting these side‑effects are cumulative and can impair adherence more than the occasional headache from a nitrate. Sixth, the drug’s metabolic pathway via CYP2D6 introduces genotype‑driven variability, which is rarely screened for in primary care, leading to unpredictable plasma concentrations. Seventh, the claim of negligible impact on blood pressure is contingent on the absence of concurrent antihypertensives that could mask subtle hemodynamic shifts. Eighth, the therapeutic ceiling is not well defined; clinicians often titrate to the highest tolerated dose without clear evidence of incremental efficacy beyond 1000 mg BID. Ninth, the real‑world data suggest a modest 10–15% relative risk reduction in angina frequency, which may not justify the added complexity for many patients already optimized on beta‑blockers or calcium‑channel blockers. Tenth, drug‑drug interaction checkers frequently flag Ranolazine for a litany of agents, complicating polypharmacy in the elderly. Eleventh, the lack of head‑to‑head trials against newer agents like ivabradine leaves a knowledge gap that guideline committees fill with expert opinion rather than robust evidence. Twelfth, the post‑marketing surveillance reports hint at rare but serious hepatic injury, a signal that is swallowed under the broader safety narrative. Thirteenth, the reliance on QT monitoring creates logistical hurdles for patients in rural settings lacking ready ECG access. Fourteenth, insurers often demand prior authorization, adding an administrative barrier that can delay therapy initiation. Fifteenth, the overarching message is that Ranolazine is a niche tool, not a universal solution, and its deployment should be predicated on a rigorous, individualized risk‑benefit assessment rather than blanket endorsement.
Max Rogers
Just a quick grammar note: the article switches between "Ranexa" and "Ranolazine" without consistent italics. It would read cleaner if drug names were consistently formatted, and bullet points could use semicolons for a smoother flow.
Louie Hadley
Hey everyone, let’s keep it civil. Both old and new meds have pros and cons, and the best pick depends on the patient’s full picture. No need to demonize any class.
Carys Jones
Honestly, pushing a $120 drug when cheaper beta‑blockers exist feels like a money grab. Patients deserve transparency about cost versus benefit.
Roxanne Porter
From a formal standpoint, the comparative table could benefit from clearer headings and a uniform font size to improve readability for clinicians.
Jonathan Mbulakey
The suggestion to standardize headings aligns with best practices in medical writing; consistency aids rapid information retrieval, especially under time pressure.
Warren Neufeld
I understand the concerns about QT monitoring; for many patients the burden is worth the relief from daily chest pain. Empathy for both sides is key.
Hoyt Dawes
Another lazy take: the article pretends Ranolazine is a miracle without acknowledging the stubborn reality that most patients never reach perfect symptom control.
Fiona Doherty
Calling it a "miracle" is a stretch; the data show modest outcomes at best, and the hype does little for informed decision‑making.
Neil Greer
Good point about modest outcomes. I think adding a section on patient‑reported outcome measures would round out the analysis nicely.
Fionnuala O'Connor
Adding patient‑reported outcomes would indeed give a fuller picture and help clinicians weigh QoL benefits against risks.
Adam O'Rourke
Sure, but remember that patient‑reported scales are often biased by expectation; a drug marketed heavily can inflate perceived benefit.
Mary-Pat Quilty
From a cultural perspective, it’s fascinating how drug adoption varies across regions; some countries still favor older nitrates despite newer data.
Patrick McGonigle
I concur; regional guidelines often lag behind the latest evidence, emphasizing the need for continual education among practitioners.
Keisha Moss Buynitzky
In light of the evidence presented, it is prudent to adopt a shared decision‑making approach, ensuring patients are fully apprised of both therapeutic benefits and potential hazards.
Shivam yadav
Absolutely, involving patients in the conversation builds trust and often leads to better adherence to the chosen regimen.
pallabi banerjee
Ultimately, a balanced, patient‑centric strategy that respects individual preferences while grounding choices in solid data will serve everyone best.





Write a comment