
When your doctor prescribes a medication, you might see a brand name like Lyrica or Viagra on the prescription. But when you pick it up at the pharmacy, the bottle says pregabalin or sildenafil - and the price is a fraction of what you expected. That’s a generic drug. And for most people, it works just as well. But not everyone believes it. Some worry: Is the generic really the same? Could it be less safe? Worse? Even dangerous?
The truth isn’t as scary as the rumors. But it’s not simple either. Generic drugs aren’t knockoffs. They’re not cheap imitations. They’re legally required to be the same as the brand-name version - in active ingredient, strength, dosage form, and how your body absorbs it. The U.S. Food and Drug Administration (FDA) doesn’t approve them unless they pass strict tests. And yet, stories still circulate. Someone switched from brand-name Synthroid to generic levothyroxine and their TSH levels went wild. Another person on Keppra had seizures after switching to generic levetiracetam. These aren’t just online rants. They’re documented cases. So what’s going on?
What Exactly Makes a Drug "Generic"?
A generic drug must contain the exact same active ingredient as the brand-name version. That means if your brand-name drug has 10 mg of sertraline, the generic has 10 mg of sertraline - no more, no less. It must also match the brand in strength, how it’s taken (pill, liquid, injection), and how it’s absorbed by your body. This last part is critical. It’s called bioequivalence.
To prove bioequivalence, the FDA requires studies with 24 to 36 healthy volunteers. These studies measure how much of the drug enters your bloodstream (AUC) and how fast it peaks (Cmax). The generic’s numbers must fall within 80% to 125% of the brand’s. That might sound like a wide range, but it’s not. It’s based on decades of data showing that within this range, the clinical effect is essentially identical. For most drugs, this works perfectly.
There are exceptions. For drugs with a narrow therapeutic index - meaning the difference between a helpful dose and a toxic one is tiny - the FDA uses tighter standards. For drugs like warfarin, levothyroxine, or phenytoin, the acceptable range is narrowed to 90% to 112%. These are the drugs where switching brands can matter more. And that’s where most real-world problems occur.
Myth: Generic Drugs Are Made in Worse Factories
One of the most persistent myths is that generics are made in shoddy overseas plants. It’s easy to believe - after all, most generic drugs are made in India and China. But here’s the fact: the FDA inspects every facility that makes drugs sold in the U.S., whether it’s a brand-name maker in New Jersey or a generic maker in Hyderabad.
In 2022, 98.7% of generic drug manufacturing facilities passed FDA inspections. For brand-name facilities, it was 97.3%. That’s not a typo. Generics passed at a slightly higher rate. The FDA holds both to the same Current Good Manufacturing Practices (CGMP). The same rules. The same audits. The same penalties for violations. If a plant fails, it’s shut down - regardless of whether it makes brand-name or generic drugs.
So why do people think otherwise? Because bad news travels faster. When a plant in India gets flagged for data manipulation, the headlines scream "Generic Drug Scandal!" But when a brand-name plant in the U.S. has the same issue, it’s buried in the business section. The system is flawed - but not because generics are inferior. It’s because we expect more from the expensive brand.
Myth: Generics Don’t Work as Well
There’s a lot of data on this. A 2020 study in Nature analyzed 17 cardiovascular drugs and found that generic versions were not just as good - they were often better. After adjusting for patient factors, people on generics had fewer heart attacks, strokes, and deaths. For metformin and gliclazide, the benefit was clear and statistically significant.
But then there’s the other side. A 2017 Harvard study looked at older adults switching from brand-name blood pressure meds to generics. After the switch, ER visits and hospitalizations went up - by 8% for losartan, 12% for valsartan, 14% for candesartan. Another study found higher rates of psychiatric hospitalizations with generic escitalopram and sertraline.
So which is it? Are generics better? Worse? The answer is: it depends on the drug.
For most common medications - antibiotics, statins, blood pressure pills, antidepressants - the evidence is overwhelming: generics work just as well. But for a small group of drugs - especially those with narrow therapeutic windows - switching can cause problems. The difference isn’t in the active ingredient. It’s in the inactive ones. Fillers, dyes, binders. These don’t treat your condition. But they affect how the drug dissolves in your stomach. For a drug like levothyroxine, even a tiny change in absorption can throw your thyroid levels off. That’s why some patients need to stick with one manufacturer, even if it’s the brand-name version.

Myth: All Generics Are the Same
This is where things get tricky. All generics for a given drug must meet FDA standards. But they don’t all come from the same company. There might be 10 different makers of generic amlodipine. Each uses slightly different fillers, different manufacturing processes, different crystal structures. The FDA says that’s fine - as long as each batch meets bioequivalence standards.
But here’s the catch: once you’ve stabilized on one generic, switching to another - even another FDA-approved one - can cause problems. That’s why doctors sometimes recommend sticking with the same manufacturer. The FDA even says so in its guidance for narrow therapeutic index drugs.
And here’s another thing: generic labels often don’t list inactive ingredients as clearly as brand-name labels. In 2022, only 67% of generic drug labels included full details about fillers and dyes. Brand-name labels? Almost all of them - 99%. If you have a rare allergy to lactose or a dye like FD&C Red No. 40, you might not know the generic you’re taking contains it. That’s a real risk.
Why Do Some People Have Bad Experiences?
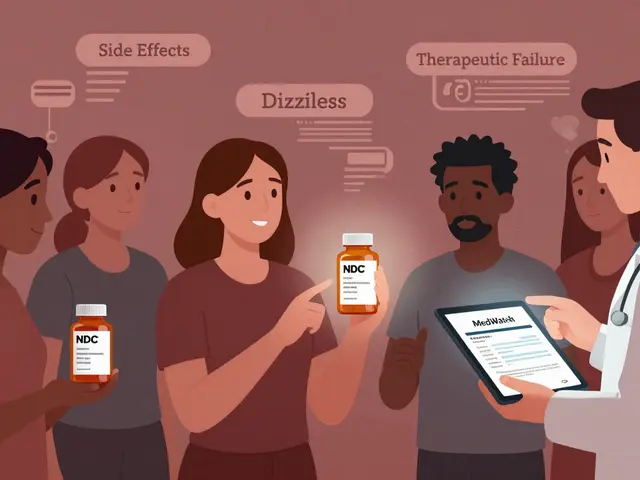
Let’s talk about real stories. One Reddit user switched from brand-name Synthroid to generic levothyroxine and spent six months adjusting their dose. Another had breakthrough seizures after switching from Keppra to generic levetiracetam. These aren’t isolated. There are documented cases where a patient’s infection didn’t clear up on generic ciprofloxacin - until they switched back to the brand.
What’s happening? Three things.
- Pharmacokinetic variation: Even within FDA limits, small differences in absorption can matter for drugs where the margin for error is slim.
- Psychological effect: If you believe the generic won’t work, your body might respond differently. Placebo and nocebo effects are real - especially with chronic conditions.
- Switching too often: If your pharmacy switches you between different generic brands every refill, your body never gets a chance to stabilize. That’s a system problem, not a drug problem.
For most people, none of this matters. But for those on thyroid meds, epilepsy drugs, blood thinners, or certain psychiatric medications - consistency matters. If you’ve been stable on a brand-name drug, don’t switch unless your doctor advises it. If you’re on a generic and feel off, don’t assume it’s "all in your head." Talk to your doctor. Get your levels checked. Sometimes, going back to the original brand - even if it costs more - is the right choice.
What Should You Do?
You don’t need to fear generics. You need to be smart about them.
- For common conditions: High blood pressure, cholesterol, diabetes, infections - generics are safe, effective, and save you money. Use them without hesitation.
- For narrow therapeutic index drugs: Levothyroxine, warfarin, phenytoin, cyclosporine, digoxin - talk to your doctor before switching. Ask if you can stick with one manufacturer. If you’re stable, don’t change.
- Check the label: Look at the inactive ingredients. If you’re allergic to something, ask your pharmacist to verify.
- Don’t let your pharmacy switch brands randomly: If your prescription says "dispense as written," they can’t substitute without your permission. Ask for it if you’re on a sensitive drug.
- Track how you feel: Keep a simple journal. Note your energy, mood, symptoms, side effects. If something changes after a switch, document it. Bring it to your doctor.
Generic drugs saved the U.S. healthcare system over $2 trillion in the last decade. They’re not perfect. But they’re not the enemy. The real issue isn’t the drugs - it’s the lack of transparency and inconsistent switching. The system needs to improve. But you don’t have to wait for it to fix itself.
Know your meds. Ask questions. Don’t assume. And don’t let fear stop you from saving money - unless you’re one of the small group for whom it matters.
Frequently Asked Questions
Are generic drugs as safe as brand-name drugs?
Yes, for the vast majority of drugs. The FDA requires generic drugs to meet the same safety, strength, quality, and purity standards as brand-name drugs. They’re held to the same manufacturing rules and inspected using the same criteria. The only real safety difference comes from inactive ingredients - like dyes or fillers - which can affect people with rare allergies. But the active ingredient, the part that treats your condition, is identical.
Why do some people say generics don’t work for them?
For most people, they do. But for a small number - especially those on drugs with a narrow therapeutic index like levothyroxine, warfarin, or seizure medications - even tiny differences in how the drug is absorbed can cause problems. These differences come from inactive ingredients or manufacturing variations, not the active drug. Also, switching between different generic brands too often can disrupt stability. Psychological factors and the nocebo effect (expecting something to fail) can also play a role.
Can I switch between different generic brands?
For most drugs, yes - and it’s often done automatically by pharmacies to save money. But for drugs like thyroid meds, blood thinners, or epilepsy treatments, switching between manufacturers can cause your levels to fluctuate. If you’re stable on one generic, it’s safer to stick with it. Ask your doctor or pharmacist to note "dispense as written" on your prescription if you’re on a sensitive medication.
Do generic drugs have the same side effects?
The side effects from the active ingredient are the same. But you might experience new or different side effects if you’re sensitive to an inactive ingredient - like a dye, preservative, or filler - that’s different in the generic version. If you notice new symptoms after switching, check the label for unfamiliar ingredients and talk to your pharmacist.
How do I know if my generic drug is FDA-approved?
All legally sold generic drugs in the U.S. must be FDA-approved. You can check the FDA’s online "Orange Book," which lists all approved generic drugs and their brand-name equivalents. If your pharmacy is licensed and you bought it in the U.S., it’s approved. If you’re unsure, ask your pharmacist to show you the label or confirm the manufacturer is on the FDA’s list.
Joie Cregin
Just wanted to say I switched my mom from brand-name Synthroid to generic last year after her insurance dropped coverage. She was terrified, but her doctor monitored her TSH closely and we didn’t notice a single change. She’s got more money for groceries now, and that’s a win.
Not everyone’s the same, but for most of us, it’s not a battle worth fighting.
john Mccoskey
Let’s cut through the noise. The FDA’s bioequivalence range of 80-125% is a joke wrapped in regulatory paperwork. That’s a 45% swing in absorption - that’s not ‘equivalent,’ that’s a crapshoot. If your drug has a narrow therapeutic index, you’re playing Russian roulette with your health. The fact that this is even allowed is a scandal disguised as cost-saving.
And don’t get me started on the factories. Sure, the FDA inspects them, but inspections are scheduled, not random. You think a plant in India is going to risk their entire production line just because some inspector’s coming next week? Of course not. They clean up the paperwork, cook the data, and go back to business as usual. The system isn’t broken - it’s designed to look like it works while letting corporations profit off your body.
Generics aren’t the enemy. The profit-driven, regulatory-captured healthcare system is. And until we stop treating medication like a commodity, people will keep getting sick because someone’s spreadsheet said ‘it’s close enough.’
brooke wright
I had a seizure after switching to generic levetiracetam and no one would believe me until I brought my blood levels in - they were half of what they were on the brand. My neurologist said it was ‘probably placebo’ until I showed him the lab report. Now I have a note on my file that says ‘DO NOT SUBSTITUTE.’
Don’t let anyone tell you your experience isn’t real. Your body knows.
Ryan Hutchison
India makes generics? Big deal. We used to make everything here. Now we outsource everything and then panic when it doesn’t work. We’re not a nation anymore - we’re a customer service line with a pharmacy.
Meanwhile, China’s building railroads and we’re debating whether a filler in a pill is ‘safe enough.’ Pathetic. At least the generics are cheap. That’s the only thing keeping this dumpster fire from collapsing.
evelyn wellding
Just wanted to say THANK YOU for this post!! 😊 I was so scared to switch my antidepressant but now I feel way more informed. I’m sticking with one generic brand and checking the label like you said. Small steps, right? 💪
Melodie Lesesne
I’m a pharmacist and I see this every day. Most people don’t realize that when you switch between generic manufacturers, it’s like switching from one brand of coffee to another - same beans, different roast. For most drugs, it’s fine. But for thyroid meds? That’s like switching from drip to espresso. You feel it.
I always ask patients: ‘Are you feeling different?’ If they say yes, we go back to the original. No shame in that. Health isn’t a spreadsheet.
Samyak Shertok
Oh wow, so the FDA says it’s fine, but then you have people having seizures? How is this not a crime? I mean, seriously - if your car’s engine had a 45% variance in fuel delivery, you’d sue the manufacturer. But when your brain’s chemistry is at stake? ‘Oh, it’s within range.’
And let’s not pretend the ‘inactive ingredients’ are harmless. That’s like saying the poison isn’t in the apple, it’s in the wax. Wake up. This isn’t science - it’s corporate math.
Nick Cole
My wife’s on warfarin. We’ve been on the same generic for 4 years. No issues. But when the pharmacy switched her to a different maker last year? INR spiked. We almost ended up in the ER.
It’s not about brand vs generic. It’s about consistency. Once you find a version that works, lock it in. And if your pharmacist tries to swap it without asking - say no. Loudly.
Chelsea Harton
generic is fine unless you’re on thyroid or seizure meds. then just stick with one. and check the label. its not that hard.
Joie Cregin
I’m so glad you said that about the label. I didn’t realize generics often leave out the dye info. My sister’s allergic to FD&C Red No. 40 - she broke out in hives every time she got a new bottle until we started checking the inactive ingredients. Now we print them out and keep them in her med organizer.
It’s ridiculous we have to be detectives just to stay safe.
Corey Chrisinger
It’s funny how we trust the FDA to regulate our food, our air, our water - but when it comes to medicine, we treat it like a lottery. Maybe we’ve been conditioned to believe that expensive = better. But the truth? The pill in the $4 generic and the $150 brand have the same soul.
The difference is in the packaging. And the profit margin.
What if we stopped seeing drugs as products and started seeing them as part of our collective health? Would we still let corporations decide what’s ‘close enough’?
Rob Deneke
Just because you’re on a narrow therapeutic index drug doesn’t mean you’re doomed. Talk to your doctor. Get tested. Stay consistent. You got this. Your health is worth the extra step.
And hey - if your insurance tries to force a switch? Say no. They can’t override your doctor’s order. You’re not powerless.
Travis Craw
my doc told me to switch to generic and i did. felt weird for a week. thought it was me. then i switched back and felt normal again. so now i just ask for the brand every time. its more expensive but i dont wanna risk it.
also i dont trust the pharmacy to remember what i need. they always mix it up.




Write a comment