
When you’re pregnant or breastfeeding, every pill, supplement, or over-the-counter remedy matters more than ever. What seemed harmless before could now affect your baby’s development, your milk supply, or your own health in ways you didn’t expect. That’s why talking openly and clearly with your OB/GYN about everything you’re taking isn’t just a good idea-it’s essential.
Why Medication Talks with Your OB/GYN Are Different
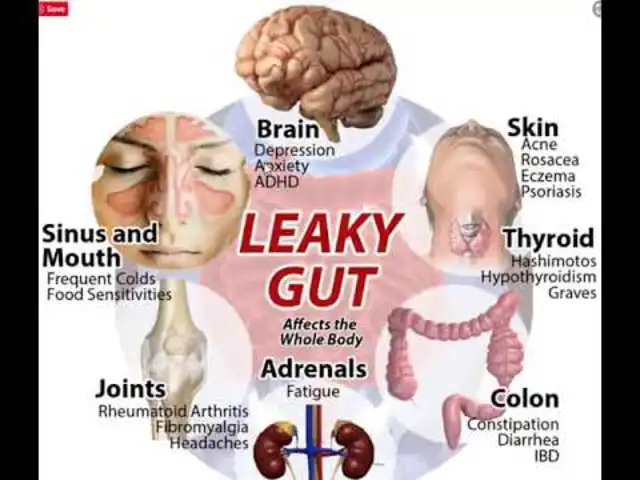
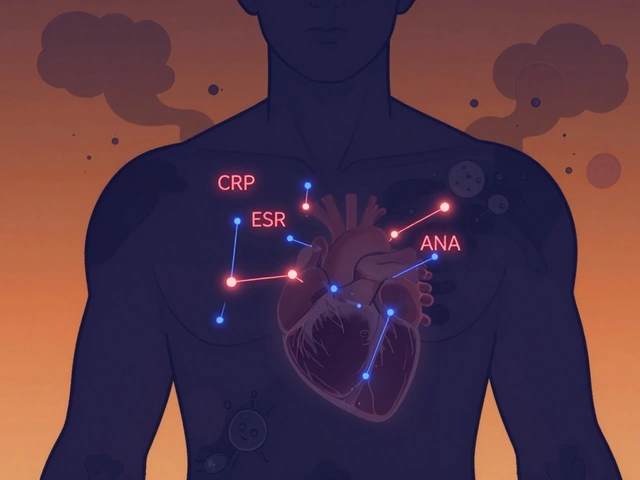
Most doctors review your meds once a year. Your OB/GYN? They need to know what you’re taking every time you walk in-especially if you’re trying to get pregnant, already pregnant, or nursing. Why? Because your body’s chemistry changes dramatically during these phases. A drug that’s perfectly safe for a 35-year-old man might be risky for a pregnant woman in her first trimester. The American College of Obstetricians and Gynecologists (ACOG) says all medications-prescription, over-the-counter, herbal, and even supplements-must be reviewed during prepregnancy visits. And it’s not just about avoiding harm. Many chronic conditions like high blood pressure, thyroid issues, or depression need careful management during pregnancy. Stopping the wrong medication can be just as dangerous as continuing the wrong one. For example, if you take Synthroid for hypothyroidism, your dose may need to increase by 25-50% during pregnancy. If you’re on ibuprofen for migraines, it could affect your baby’s kidney function after 20 weeks. And if you’re taking St. John’s Wort for low mood, it can cut the effectiveness of birth control pills by half. These aren’t edge cases-they’re common.What to Bring to Your Appointment
Don’t rely on memory. Write it down. Here’s exactly what to include:- Prescription meds: Name, dose, how often, and why you take it. Example: “Levothyroxine 75 mcg, one tablet daily for hypothyroidism.”
- Over-the-counter drugs: Even if you only take them occasionally. That Advil you use for headaches? List it. The melatonin you take to sleep? List it too.
- Supplements and vitamins: Brand names matter. “Nature Made Prenatal” is different from “Garden of Life.” Include dosage: “1 capsule daily.”
- Herbal products: Turmeric, ginger tea, evening primrose oil, red raspberry leaf-yes, even these. Many women think “natural” means safe. It doesn’t.
- Recreational substances: Alcohol, nicotine, cannabis. If you use them, even once a week, say so. Your OB/GYN isn’t here to judge-they’re here to help you stay safe.
How to Organize Your List
Keep it simple. Use your phone’s notes app or print a sheet. Include:- Medication name (generic and brand, if different)
- Dosage (e.g., 500 mg, 10 mg, 1 tablet)
- Frequency (daily, twice a day, as needed)
- Reason you take it
- When you last took it

Questions to Ask Your OB/GYN
Come prepared with questions. Here are the top ones patients should ask:- “Is this medication safe during pregnancy or breastfeeding?”
- “Are there safer alternatives?”
- “Should I stop taking this before trying to conceive?”
- “Will this affect my fertility or my baby’s development?”
- “What happens if I miss a dose?”
- “Is this drug on the FDA’s pregnancy risk list? What category is it?”
What Your OB/GYN Won’t Tell You (But Should)
Many providers focus on big-ticket drugs-antidepressants, blood pressure meds, diabetes pills. But they often miss the small stuff. St. John’s Wort, kava, dong quai, and even high-dose vitamin A can interfere with pregnancy or fetal development. A 2020 study in Pharmacotherapy found that 50% of women on oral contraceptives who took St. John’s Wort had unintended pregnancies. Cannabis is another blind spot. The National Survey on Drug Use and Health (2022) found 18% of reproductive-aged women use medical marijuana. But only 38% of OB/GYNs routinely screen for it. If you use CBD or THC for anxiety, pain, or nausea, say so. It can affect placental function and fetal brain development. And don’t assume your OB/GYN knows everything. Many don’t. That’s why some practices now refer complex cases to women’s health pharmacists. If you take four or more medications, ask if a pharmacist consultation is available. It’s free through many insurance plans.What to Do After the Appointment
Don’t walk out with more questions than answers. If your OB/GYN says, “We’ll switch you to this,” ask for written instructions. Get the new drug’s name, dose, and when to start. If they say, “Stop this,” ask: “When exactly? Right away? After 2 weeks? After the first trimester?” Update your list. Keep it on your phone. Share it with your partner or a trusted friend. If you’re switching meds, set a reminder to check in with your OB/GYN in 2-4 weeks. Hormonal changes can shift how your body handles drugs-what worked last month might need adjusting now.
Common Mistakes and How to Avoid Them
- Mistake: “I didn’t think it counted.” Solution: Everything counts. Even a daily ginger tea.
- Mistake: “I forgot.” Solution: Keep your list in your wallet or phone case. Review it every Monday.
- Mistake: “I’m scared they’ll think I’m overdoing it.” Solution: Your OB/GYN has seen it all. Honesty saves lives.
- Mistake: “I’ll just Google it.” Solution: Google is full of misinformation. Trust your provider’s guidance-not a blog post.
When to Start Preparing
If you’re thinking about getting pregnant, start now. Not next month. Not when you miss your period. Start today. ACOG recommends reviewing all medications at least three months before conception. That gives time to safely switch out risky drugs, adjust doses, or begin folic acid (400-800 mcg daily) to prevent neural tube defects. If you’re already pregnant, don’t wait for your next appointment. Call your OB/GYN’s office and ask for a medication review. Many clinics now offer virtual consults just for this purpose.Final Thought: This Is Your Health, Too
Pregnancy and breastfeeding aren’t just about your baby. They’re about you. You deserve to feel safe, supported, and informed. You’re not being difficult for asking questions. You’re being smart. The system isn’t perfect. Many OB/GYNs are rushed. Insurance limits what they can prescribe. But you hold the power: you bring the list. You ask the questions. You follow up. That’s how you turn a 15-minute check-in into a life-changing conversation.Can I keep taking my antidepressants while pregnant?
Some antidepressants, like sertraline (Zoloft) and citalopram (Celexa), are considered low-risk during pregnancy and are often continued under supervision. Others, like paroxetine (Paxil), are linked to a slightly higher risk of heart defects and are usually avoided. Never stop abruptly-withdrawal can cause serious symptoms. Always work with your OB/GYN and a psychiatrist to weigh risks and benefits.
Is it safe to take ibuprofen while breastfeeding?
Yes, ibuprofen is generally considered safe during breastfeeding. Only tiny amounts pass into breast milk, and studies show no negative effects on infants. It’s often preferred over naproxen or aspirin. But avoid it during pregnancy after 20 weeks-it can affect fetal kidney development and reduce amniotic fluid.
What if I took a medication before I knew I was pregnant?
Don’t panic. Most medications taken in the first two weeks after conception either have no effect or cause an all-or-nothing outcome-if the embryo is damaged, it won’t survive. If you’re past that window, your OB/GYN will assess the specific drug, timing, and dose. Many common meds (like antibiotics or acetaminophen) pose little to no risk. Document everything and let your provider help you evaluate it.
Are herbal teas safe during pregnancy?
Some are, some aren’t. Ginger and peppermint tea are generally fine in moderation. But red raspberry leaf can stimulate contractions and is often avoided in early pregnancy. Chamomile may affect hormone levels, and licorice root can raise blood pressure. Always check with your OB/GYN before drinking any herbal tea regularly.
Why does my OB/GYN care about my birth control if I’m trying to get pregnant?
Because some birth control methods affect how your body responds after stopping. For example, the Depo-Provera shot can delay ovulation for up to 10 months. Hormonal IUDs may cause thinning of the uterine lining. Knowing what you used helps your provider predict when you might conceive and adjust prenatal care timing accordingly.
Melissa Taylor
Just had my 20-week scan and brought my full med list like the article said. The nurse actually printed it out and stapled it to my chart. Felt so seen. This stuff matters.
John Brown
Been doing this since my first preg. Writing it down saves everyone time. My OB once asked if I was a pharmacist because my list was so clean. I told her I just didn’t want my baby to get hurt by a typo.
Benjamin Glover
Most Americans have no idea how to manage basic health. This article reads like a kindergarten handbook for adults.
Raj Kumar
Bro, I took ashwagandha for stress and didn't think it counted. Then my doc said it might mess with thyroid levels. Wild. Now I list everything-even the turmeric lattes. Learned the hard way.
Jocelyn Lachapelle
My OB told me to stop my magnesium supplement because it might trigger contractions. I didn't know that. Now I check every single thing. Even the tea bags.
RONALD Randolph
There is no excuse for not having a written, organized, time-stamped, medication log-especially when your child’s life is on the line! If you can’t manage this, you shouldn’t be having children!
Christina Bischof
My partner made me a spreadsheet with icons for each med-green for safe, yellow for caution, red for stop. We printed it. I cried. It felt like someone finally got it.
Cassie Henriques
So I asked my doc about CBD for nausea and she said it’s Category C. I had no idea what that meant. Then she pulled up the FDA chart and explained it like I was 10. Best. Appointment. Ever. 🤓
Jake Sinatra
It is imperative that expectant mothers recognize the gravity of pharmacological intervention during gestation. The physiological adaptations of pregnancy necessitate a rigorous, evidence-based approach to therapeutic management. This article provides an exemplary framework for patient-provider collaboration.
Mike Nordby
I’ve been a nurse for 18 years. I’ve seen women stop their blood pressure meds because they heard it ‘hurts the baby.’ I’ve seen others keep taking opioids because they were scared to ask. This article is the bare minimum. We need more of this.
John Samuel
Imagine walking into a room where your life, your baby’s life, and your sanity hang in the balance-and you’re expected to remember every pill, potion, and herbal elixir you’ve ever consumed since 2019. This isn’t just advice-it’s a lifeline wrapped in a spreadsheet. Bravo.
Sai Nguyen
Why are we letting women take so many things? In my country, we just avoid all meds. Simple. Clean. Safe.




Write a comment