MAOI Drug Interaction Checker
Check if Your Medications Are Safe Together
This tool helps determine if your current antidepressant is safe to combine with MAOIs. Always consult your psychiatrist before making medication changes.
Important Safety Information
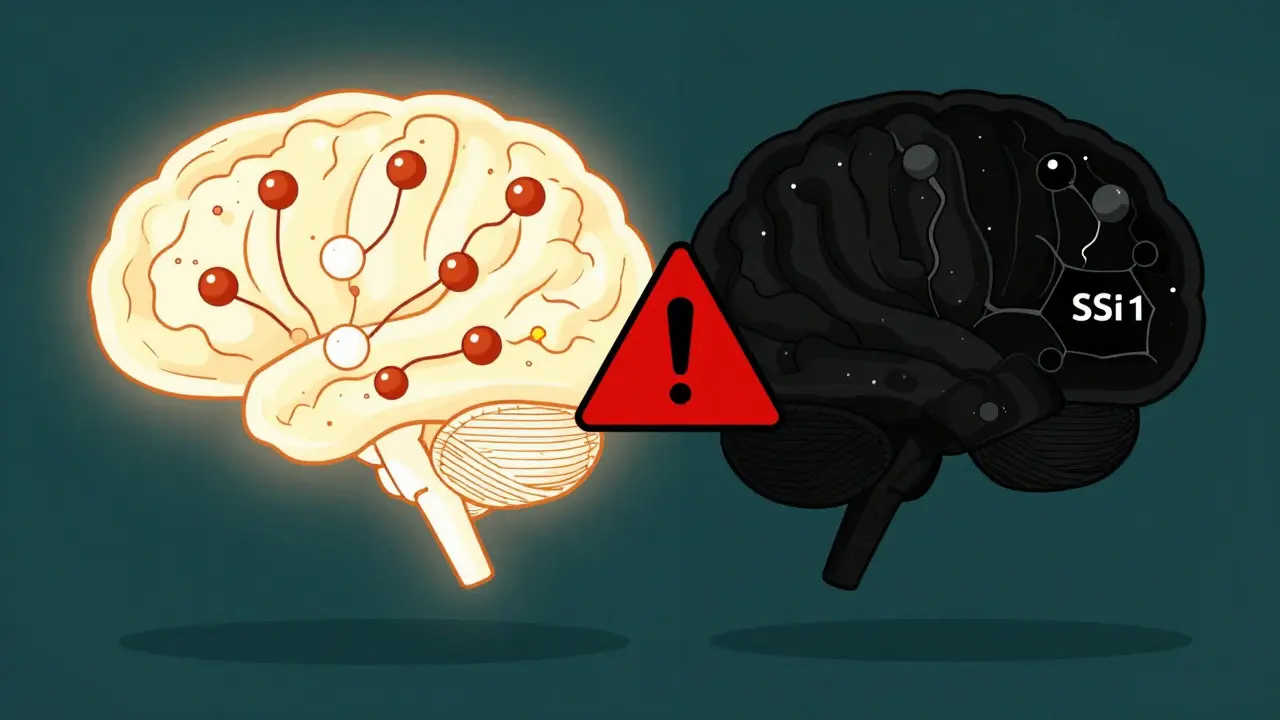
Combining MAOIs with certain antidepressants can cause serotonin syndrome - a potentially fatal condition.
Signs of serotonin syndrome include:
- High fever
- Muscle rigidity
- Rapid heart rate
- Confusion or agitation
- Sweating, shivering, or diarrhea
If you experience these symptoms after starting or changing antidepressants, seek emergency medical care immediately.
Why MAOIs Are Still Used Despite the Risks
MAOIs aren’t the first drug you think of when someone says "antidepressant." They’re old, they come with warnings that scare even experienced doctors, and you have to avoid certain foods like aged cheese and draft beer. But for some people-those who’ve tried every other antidepressant and still feel stuck-they’re the only thing that works. Around 20 to 30% of people with depression don’t respond to standard treatments. These are called treatment-resistant cases. For them, MAOIs like phenelzine, tranylcypromine, and the selegiline patch can make the difference between surviving and sinking.
MAOIs work differently than SSRIs or SNRIs. Instead of blocking serotonin reuptake, they stop the enzyme that breaks down serotonin, norepinephrine, and dopamine. That means more of these mood-lifting chemicals stay active in the brain. It’s not just about lifting sadness-it helps with the heavy, numb feeling called "leaden paralysis," the oversleeping, the intense fear of rejection. These are symptoms that often don’t improve with fluoxetine or sertraline.
The catch? These drugs are powerful, and mixing them with other antidepressants can be deadly.
The Deadly Mix: MAOIs and SSRIs/SNRIs
Combining MAOIs with SSRIs like fluoxetine, sertraline, or escitalopram isn’t just risky-it’s dangerous. The result can be serotonin syndrome: a medical emergency where your body overheats, your muscles lock up, your heart races, and your mind goes confused or agitated. In extreme cases, it kills.
A 1995 study in the Journal of Clinical Psychiatry looked at eight cases where people took fluoxetine and tranylcypromine together. Seven ended in death. That’s not a fluke. The FDA requires a boxed warning on every MAOI label: do not combine with SSRIs or SNRIs.
It’s not just about taking them at the same time. Timing matters. If you stop an SSRI, you can’t start an MAOI right away. For most SSRIs, you need to wait 14 days. But fluoxetine? That’s different. It sticks around in your system for weeks because its metabolite, norfluoxetine, lasts even longer. You need a full five weeks before switching to an MAOI. Go too soon, and your brain is still flooded with serotonin. The MAOI then stops the cleanup crew. The result? Toxic buildup.
And if you’re switching the other way-MAOI to SSRI? Same rule. Wait 14 days after stopping the MAOI. Your body needs time to rebuild the enzyme that breaks down serotonin. Jump the gun, and you’re playing Russian roulette with your nervous system.
The Gray Area: MAOIs and Tricyclic Antidepressants
Here’s where things get messy. For years, doctors were told: never mix MAOIs with TCAs like amitriptyline or clomipramine. The theory was simple-both increase serotonin. Too much = danger.
But recent research is challenging that. A 2022 review in PMC9680847 found that when done right, combining MAOIs with certain TCAs can actually help people who’ve run out of options. The key? It’s not about mixing any TCA with any MAOI. It’s about which one, and how you do it.
Clomipramine? Never combine it with an MAOI. It’s too strong on serotonin. But nortriptyline? That’s a different story. Studies by Dr. J. David Amsterdam showed that 57% of treatment-resistant patients improved when phenelzine was added to nortriptyline-with few serious side effects. The trick? Start the TCA first. Or start both at the same time. Never add the MAOI after the TCA is already running. That’s when the risk spikes.
Still, most guidelines, including the FDA and Mayo Clinic, say it’s contraindicated. But some psychiatrists who specialize in treatment-resistant depression are quietly using this combo-carefully, slowly, with close monitoring. It’s not for beginners. It’s not for general practitioners. It’s for specialists who know the signs of trouble and have the patience to titrate doses over weeks.
Safer Combinations: What You Can Actually Mix
If you’re on an MAOI and still struggling, you don’t have to give up. There are antidepressants that play nicely with MAOIs. They don’t boost serotonin the same way. They work on other pathways.
Bupropion is one of the safest. It targets dopamine and norepinephrine, not serotonin. No serotonin overload. No serotonin syndrome risk. Multiple case reports and expert reviews, including from Dr. Kenneth Heilman, support its use alongside MAOIs for patients with low energy or lack of motivation.
Mirtazapine works differently too. It blocks certain receptors that suppress mood, and it doesn’t inhibit serotonin reuptake strongly. Studies from the University of Michigan and the Psychotropical journal show it can be added safely to MAOIs for patients with insomnia or poor appetite. It even helps with sleep without the dependency risk of benzodiazepines.
Trazodone is another option. Used often for sleep, it has minimal effect on serotonin reuptake at low doses. It’s commonly paired with MAOIs in clinical practice for patients who can’t sleep and feel emotionally numb.
And then there’s nortriptyline, which we mentioned earlier. While it’s a TCA, its lower serotonergic activity makes it a rare exception. It’s not first-line, but for stubborn cases, it’s one of the few TCAs that can be used with MAOIs-under expert supervision.
Other Tools: What Else Can You Add?
Antidepressants aren’t the only tools. Sometimes you need help with anxiety, sleep, or focus. The good news? Many of those medications are safe with MAOIs.
Benzodiazepines like lorazepam or clonazepam? Fine. They don’t affect serotonin. They help with panic, agitation, or insomnia without adding risk. Sleep aids like zolpidem or suvorexant? Also safe. No interaction.
Even dopamine-targeting drugs like pramipexole (used for Parkinson’s) can help with the deep apathy and anhedonia that MAOIs alone don’t always fix. Case reports from Yale and the University of Pennsylvania show patients who couldn’t feel joy started responding again when pramipexole was added. It takes slow dosing-start low, go slow-to avoid nausea or dizziness. But it works.
And if you’re dealing with chronic pain alongside depression? MAOIs can help with that too. They’re one of the few antidepressants that ease nerve pain. That’s why they’re sometimes used for fibromyalgia or diabetic neuropathy.
Dietary Restrictions: Still a Big Deal
Even with newer patches like Emsam, diet still matters. Tyramine-a compound in aged, fermented, or spoiled foods-can cause dangerous spikes in blood pressure when MAOIs are active in your system.
Aged cheeses (cheddar, blue, parmesan), tap beer, soy sauce, fermented meats like salami or pepperoni, and even overripe bananas or fava beans can trigger a hypertensive crisis. Symptoms? Severe headache, blurred vision, chest pain, rapid heartbeat. It can lead to stroke or heart attack.
The transdermal selegiline patch at 6mg/24hr reduces this risk. Most people on this dose don’t need to change their diet. But if you’re on oral MAOIs like phenelzine or tranylcypromine? You still need to avoid those foods. And you need to keep avoiding them for two weeks after you stop the MAOI. Your enzyme levels don’t snap back instantly.
Stopping MAOIs: Don’t Just Quit
Stopping an MAOI cold turkey is a bad idea. You don’t just lose the benefit-you get withdrawal symptoms that feel like a bad flu mixed with anxiety.
One 2004 study found that 71% of people who stopped abruptly had sleep problems. 68% got headaches. 62% felt restless. 55% had flu-like symptoms. 48% had stomach upset. And 37% felt tingling or burning skin.
Always taper. Slowly. Over two to four weeks. Your doctor should guide you. Don’t reduce your dose by half each week. Try cutting 10-25% every 5-7 days. Keep track of how you feel. If symptoms flare up, slow down.

Who Should Be Prescribing This?
Only about 5-10% of depression specialists regularly prescribe MAOIs today. Why? Because most doctors don’t know how to use them safely. A 2019 study found only 32% of psychiatry residents felt confident managing MAOI interactions.
These aren’t drugs for primary care. They’re for specialists-psychiatrists who’ve seen treatment-resistant cases before, who know the signs of serotonin syndrome, who’ve read the old papers and the new ones. If your doctor pushes you toward an MAOI, ask: "Have you prescribed this before? Have you managed combinations?" If they hesitate, get a second opinion.
The Future: Where MAOIs Are Headed
MAOIs aren’t going away. They’re being refined. The selegiline patch is just the beginning. Researchers are testing selective MAO-B inhibitors that avoid dietary issues entirely. There’s even early work combining MAOIs with ketamine for rapid relief in suicidal depression.
But for now, the real power of MAOIs lies in their precision. They’re not for everyone. But for the 15-20% of people who’ve tried everything else? They’re often the only thing left that works. The key isn’t avoiding them. It’s using them right-with knowledge, patience, and expert oversight.
When to Consider an MAOI
- You’ve tried at least two antidepressants from different classes (SSRI, SNRI, TCA) with no improvement
- You have atypical depression symptoms: oversleeping, heavy limbs, rejection sensitivity
- You’re struggling with severe anhedonia or apathy that other meds don’t touch
- You’re under the care of a psychiatrist experienced with MAOIs
- You’re willing to follow dietary rules and avoid risky drug combinations
When to Avoid MAOIs
- You’re currently on an SSRI, SNRI, or clomipramine
- You’ve taken fluoxetine in the last five weeks
- You have uncontrolled high blood pressure
- You’re not ready to change your diet or avoid certain medications
- Your doctor hasn’t treated MAOIs before
Can I take an MAOI if I’ve been on Prozac?
No, not without waiting at least five weeks after your last dose. Prozac (fluoxetine) and its active metabolite stay in your system for weeks. Starting an MAOI too soon can cause serotonin syndrome, which can be fatal. Always confirm washout periods with your psychiatrist.
Is it safe to combine MAOIs with Wellbutrin?
Yes, bupropion (Wellbutrin) is one of the safest antidepressants to combine with MAOIs. It doesn’t affect serotonin reuptake significantly, so it doesn’t raise the risk of serotonin syndrome. Many psychiatrists use this combo for patients with low energy, lack of motivation, or attention problems.
Can I eat cheese while on an MAOI?
If you’re taking an oral MAOI like phenelzine or tranylcypromine, avoid aged cheeses, tap beer, fermented meats, and soy sauce. These contain tyramine, which can spike your blood pressure dangerously. If you’re on the selegiline patch at 6mg/24hr or lower, dietary restrictions are usually not needed. Always check with your doctor based on your dose and formulation.
What are the signs of serotonin syndrome?
Symptoms include high fever, muscle rigidity, rapid heart rate, confusion, agitation, sweating, shivering, and diarrhea. If you experience these after starting or changing antidepressants, seek emergency care immediately. Serotonin syndrome can progress quickly and become life-threatening.
Why aren’t MAOIs used more often?
Because they’re complex to use safely. Many doctors lack training in managing drug interactions, dietary restrictions, and withdrawal. The fear of serotonin syndrome and hypertensive crises makes them hesitant. But for treatment-resistant depression, they remain one of the most effective tools-if used correctly.
MAOIs aren’t a first-line fix. They’re a last-resort option that works when everything else fails. But that doesn’t make them outdated. It makes them essential. The key isn’t avoiding them-it’s knowing when, how, and with whom to use them. If you’re stuck in treatment-resistant depression, ask your psychiatrist: "Could an MAOI be right for me?" Don’t assume it’s too risky. Ask for the evidence. And make sure you’re being guided by someone who’s done this before.
Vatsal Srivastava
MAOIs are the only reason I'm still alive. SSRIs turned me into a zombie. This post nails it. No fluff. Just facts. And yes, I eat blue cheese. I'm not dying. Probably.
Brittany Marioni
I just want to say-thank you-for writing this with such clarity. So many people are scared of MAOIs, but they’re not monsters. They’re tools. And like any tool, they need to be used with care, knowledge, and respect. If you’re struggling, please don’t give up. There’s hope. And yes, you can eat bananas. Just not the ones that look like they’re about to explode.
Monica Slypig
This is why american medicine is broken. We got these ancient, life-saving drugs and we treat them like radioactive waste. In Russia we use MAOIs like aspirin. No one dies. People live. Stop being so scared of your own pharmacology
Becky M.
I’ve been on phenelzine for 8 years. I used to cry every day. Now I garden. I cook. I talk to my mom. The diet? Yeah it’s annoying. But it’s not the end of the world. And bupropion? Game changer. I take it with my MAOI and I can finally focus. You’re not broken. You just haven’t found the right combo yet.
Eli Kiseop
Wait so if I stop sertraline can I start an MAOI after 14 days or do I need to wait longer if I was on a high dose I think I was on 200mg and my doc said 14 but now I’m second guessing
Ellie Norris
Just wanted to add-selegiline patch at 6mg is a game changer for diet. I eat cheddar, soy sauce, even the occasional craft IPA. No issues. But if you’re on oral? Don’t risk it. I lost a friend to a hypertensive crisis. It’s not a myth. It’s real. And silent.
Marc Durocher
Honestly I used to think MAOIs were just for people who couldn’t follow basic instructions. Then I met someone who’d tried 17 meds and finally got better on phenelzine. Now I just shut up and listen. Some people need the nuclear option. And that’s okay.
larry keenan
The pharmacokinetic half-life of norfluoxetine is approximately 7–15 days, which necessitates a washout period of 5 weeks prior to initiating an MAOI. This is supported by multiple case series and is consistent with the FDA’s labeling recommendations. Failure to adhere to this protocol increases the risk of serotonin syndrome by an estimated 4.7-fold.
Nick Flake
MAOIs are the quiet heroes of psychiatry. They don’t scream for attention like ketamine or cry for TikTok fame like esketamine. They just sit there. Waiting. For the people who’ve been through hell and still haven’t found peace. I’ve seen people come back from the edge with just a patch and a little patience. It’s not magic. It’s medicine. And it’s beautiful.
Chinmoy Kumar
I’m from India and we dont talk about this much but my uncle took MAOI and lived. He ate cheese and drank beer. He said he just avoided the really old ones. Maybe the body adapts? Or maybe doctors scare us too much? I’m not saying risk it. But maybe the rules are too strict for some?






Write a comment