
Milk Thistle Drug Interaction Checker
This tool helps you understand potential interactions between your medications and milk thistle based on scientific evidence from clinical studies. Note: This is not medical advice. Always consult your healthcare provider before changing medications or supplements.
Select Your Medications
Choose medications that might interact with milk thistle's effects on liver enzymes.
Interaction Results
Important Notes
- Interactions can change after 7-10 days of milk thistle use
- High-risk medications require close monitoring (INR for warfarin)
- Do not adjust medications without consulting your doctor
Most people take milk thistle for their liver. It’s popular, widely available, and often seen as a safe, natural way to support detox or recover from alcohol, poor diet, or fatty liver. But what happens when you’re also taking prescription meds? That’s where things get tricky. Milk thistle doesn’t just sit quietly in your liver-it talks to the very enzymes that break down your drugs. And that conversation can change how your medications work, sometimes with serious results.
What’s Actually in Milk Thistle?
Milk thistle isn’t just one compound. Its power comes from silymarin, a mix of flavonolignans like silybin, silychristin, and silydianin. Most supplements contain 70-80% silymarin, with common doses between 140 mg and 420 mg daily. That’s what most clinical studies use. But here’s the catch: not all supplements are made the same. A 2022 FDA review found only 32% of milk thistle products on the market actually contained the amount of silymarin listed on the label. So even if you’re taking what you think is a standard dose, you might be getting way more-or way less-than expected.
Silybin, the most active part of silymarin, has poor absorption-only 20-50% gets into your bloodstream. That’s why some newer formulas combine it with phosphatidylcholine to boost absorption. But unless you’re buying a branded, clinically tested product, you’re flying blind.
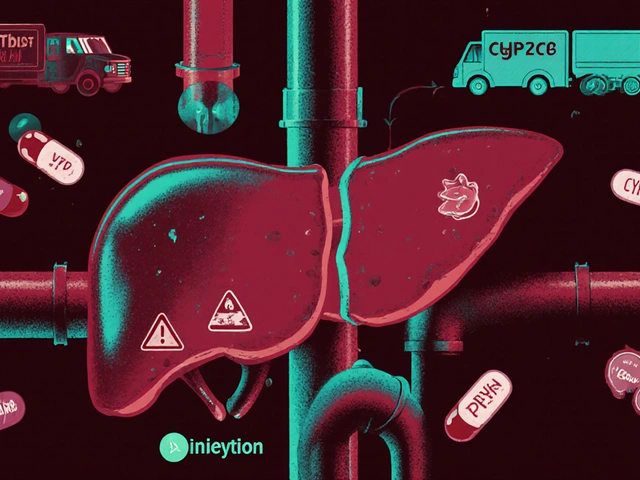
How Milk Thistle Interacts With Your Liver’s Drug-Metabolizing System
Your liver uses a family of enzymes called cytochrome P450 (CYP) to break down most medications. The big players here are CYP3A4, CYP2C9, and CYP2D6. Milk thistle doesn’t just block or boost these enzymes-it can do both, depending on how long you’ve been taking it.
Short-term use? Studies show it can inhibit CYP2C9. That means drugs processed by this enzyme-like warfarin (blood thinner), phenytoin (seizure med), and some NSAIDs-might stick around longer in your body. Higher levels. Stronger effects. Higher risk of bleeding or toxicity.
But after 7-10 days of daily use? That same study found CYP2C9 activity actually increased by over 12%. Now your body starts breaking down those drugs faster. Levels drop. The medication might stop working as well.
This flip-flop effect is why some people report no issues at first, then suddenly have problems weeks later. Or vice versa-start feeling side effects after just a few days, then they disappear. It’s not random. It’s biology.
CYP3A4, which handles about half of all prescription drugs-including statins, some antidepressants, and immunosuppressants-shows mixed results. One 2019 trial gave 420 mg of silymarin daily to healthy volunteers for two weeks. Midazolam, a drug metabolized by CYP3A4, saw only a 7.2% increase in blood levels. That’s below the 20% threshold considered clinically meaningful. So for most people, milk thistle likely won’t mess with statins or most antidepressants.
But here’s the problem: what’s true for healthy volunteers isn’t always true for someone with liver disease, older adults, or those on multiple meds. Your liver’s capacity to handle these interactions is already compromised. And genetics matter too. Some people naturally have slower or faster versions of these enzymes. That’s why two people taking the same dose of milk thistle and warfarin can have totally different outcomes.
Real-World Stories: When Theory Meets Reality
Science gives us averages. Real life gives us surprises.
On Reddit, a user posted in February 2024: “I started milk thistle for my fatty liver. Two weeks later, my INR jumped from 2.1 to 4.8. I almost bled out.” He was on warfarin. His doctor had to cut his dose by 25%. He’s not alone. In that same thread, 28 people reported needing warfarin dose changes after starting milk thistle.
Meanwhile, Amazon reviews show only 2.1% of users mention drug interactions. Most say things like “my ALT levels dropped” or “I feel less bloated.” So why the disconnect?
Because most people aren’t on warfarin. Or phenytoin. Or cyclosporine. They’re taking milk thistle for general liver support, and their meds don’t interact. But if you’re one of the minority who are, the stakes are high.
One man in Sydney, 58, with hepatitis C, took 420 mg of milk thistle daily while on sofosbuvir/velpatasvir for 12 weeks. He told Drugs.com: “No issues at all.” That matches the data-direct-acting antivirals for hepatitis C don’t seem to interact with milk thistle. But that doesn’t mean you can assume the same for your meds.

What Drugs Should You Worry About?
Not all drugs are created equal. Some have a narrow therapeutic index-meaning the difference between a helpful dose and a toxic one is tiny. These are the ones you need to be extra careful with.
- Warfarin: The biggest red flag. Even small changes in CYP2C9 activity can spike your INR. If you’re on warfarin, don’t start milk thistle without talking to your doctor-and get your INR checked weekly for the first month.
- Phenytoin: Used for seizures. Levels can drop or spike unpredictably. Monitor blood levels at days 3, 7, and 14 after starting milk thistle.
- Statins (like simvastatin, atorvastatin): Mostly metabolized by CYP3A4. Most evidence says no major interaction, but if you start feeling muscle pain or weakness, get your CK levels checked.
- Immunosuppressants (cyclosporine, tacrolimus): Used after transplants. Even small changes can lead to rejection or toxicity. Avoid milk thistle unless under strict medical supervision.
- Some antidepressants (sertraline, fluoxetine): Metabolized by CYP2D6. Data is limited, but caution is wise.
For most other medications-like blood pressure pills, thyroid meds, or insulin-there’s no strong evidence of interaction. But that doesn’t mean zero risk. Always check.
What Do Experts Really Say?
There’s a split in the medical community.
Dr. Joseph Pizzorno, a leading voice in integrative medicine, says the risk is overstated. He points to only 12 documented case reports over 40 years-and none proved causation. He argues that the benefits for liver health outweigh the unproven risks for most people.
But Dr. David S. Bernstein, a hepatologist at UConn, says otherwise. He warns that without standardized extracts and consistent data, doctors can’t predict who’s at risk. He advises caution, especially for patients on multiple drugs or with liver disease.
The European Medicines Agency says: “No clinically relevant interactions expected.” The U.S. NIH’s LiverTox database says: “Possibly interacting with CYP2C9 substrates.” That’s not a clear green light or a red flag. It’s a yellow caution sign.
And here’s the kicker: most doctors don’t know this stuff. A 2023 JAMA survey found only 28% of physicians felt confident counseling patients on milk thistle interactions-even though 64% get asked about it.

What Should You Do?
Here’s a practical step-by-step plan:
- Don’t start milk thistle without telling your doctor-especially if you’re on any prescription meds.
- Know your meds. Look up your medications on the NIH LiverTox database or ask your pharmacist. If it’s metabolized by CYP2C9 or CYP3A4, proceed with caution.
- Choose a reputable brand. Look for products that specify “70-80% silymarin” and have third-party testing (USP, NSF, or ConsumerLab seal).
- Monitor. If you’re on warfarin, phenytoin, or an immunosuppressant, get lab tests before starting and again at 7 and 14 days after starting.
- Give it time. Don’t assume an interaction will happen right away. Inhibition can start in 24-48 hours. Induction takes 7-10 days. Watch for changes in how you feel or how your meds work.
- Stop and consult if you notice unexplained bruising, dizziness, muscle pain, or changes in mood or energy.
And if you’re not on any meds that interact? Milk thistle is generally safe. Side effects are rare-only 1.2% of users in clinical trials reported anything worse than mild bloating or diarrhea. For people with fatty liver, it’s one of the few supplements with solid evidence of improving liver enzymes.
The Bigger Picture
Milk thistle is a $187 million market. It’s in 38.7% of all liver supplements sold. And it’s growing. But it’s not regulated like a drug. That means quality, dosage, and interaction risk vary wildly.
Future products might solve this. Researchers are testing silybin bound to phosphatidylcholine to improve absorption and reduce CYP interactions. Pharmacogenomic testing could one day tell you whether you’re genetically prone to metabolize silymarin in a way that affects your meds.
Until then, treat milk thistle like a drug-not a vitamin. It’s not harmless. It’s not magic. It’s a potent botanical that talks to your liver’s internal machinery. And if you’re on medications, that conversation matters.
Riohlo (Or Rio) Marie
Oh sweet mercy, another person treating botanicals like they’re harmless tea. Silymarin isn’t some gentle grandma hug for your liver-it’s a biochemical grenade with a delayed fuse. I’ve seen patients on warfarin go from INR 2.5 to 5.9 in 96 hours after ‘just trying milk thistle for detox.’ And no, the label doesn’t say ‘may cause spontaneous hemorrhage.’ Because regulation is a joke. You wouldn’t take a random pill from a street vendor and call it medicine-why treat supplements differently? This isn’t wellness culture. This is pharmacology with a side of delusion.
And don’t get me started on those ‘third-party tested’ brands. USP seal? More like ‘USP: Unverified Snake Oil Promise.’ Half of them use fillers that alter absorption kinetics. The 2022 FDA audit didn’t just find under-dosing-it found *fake* silymarin. I mean, come on. We’re letting people gamble with their liver enzymes like it’s a slot machine.
And yes, I know Dr. Pizzorno says it’s overblown. He also thinks colloidal silver cures cancer. Priorities, darling.
TL;DR: If you’re on meds, milk thistle isn’t a supplement. It’s a drug. And you’re not the first person to find out the hard way.
Also, ‘natural’ doesn’t mean ‘safe.’ It means ‘unregulated and possibly lethal.’
Conor McNamara
ok so i think this is all part of the big pharma coverup. they dont want you to know that milk thistle can fix everything but they made the FDA say its dangerous so people keep buying pills. i read on a forum that the cyp enzymes are actually controlled by satellites and milk thistle jams the signal. thats why the effect flips after 7 days. its not biology its mind control. also my cousin in dublin said he saw a guy in the park take milk thistle and then his blood turned purple. i think its real. dont trust doctors they work for the illuminati.
ps i took it for 3 days and my tummy felt weird so its working. the system is fighting back.
steffi walsh
Thank you for writing this!! I’ve been so nervous about starting milk thistle since I’m on a statin and just didn’t know who to ask. This broke it down in a way that actually made sense 😊 I’m going to talk to my pharmacist this week and get my liver enzymes checked before I even think about opening a bottle. You’re right-it’s not a vitamin, it’s a player in the game. And I’m not risking my health for a ‘feel-good’ supplement. Love that you included the step-by-step plan!! 🙌
Also, if anyone else is on simvastatin and considering it, I found a brand with USP verification and phosphatidylcholine combo. I’ll DM you the link if you want! We got this 💪
Leilani O'Neill
How is it even legal to sell this garbage? In Ireland, we don’t let people walk into pharmacies and buy snake oil labeled as ‘natural detox.’ We have standards. This is why America is falling apart-people think ‘wellness’ means they can ignore science. You don’t get to cherry-pick which laws apply to your supplements. If it interacts with warfarin, it should be prescription-only. Period.
And don’t give me that ‘but it’s herbal!’ nonsense. Plants evolved toxins to kill animals. Silymarin is no different. It’s a chemical weapon disguised as a health trend. And the fact that Amazon reviews are full of people saying ‘my bloating improved’ while ignoring the fact they nearly bled out? That’s not wellness. That’s collective stupidity.
Someone needs to sue the manufacturers. And the FDA needs to ban this until it’s proven safe. Not the other way around.
Gabe Solack
Big respect for laying this out so clearly. I’m a pharmacist in Portland and I see this exact scenario at least twice a week. Patient says ‘I started milk thistle for my fatty liver’ and then comes in with a PT/INR that’s off the charts. We’ve had two ICU transfers in the last year because of it.
Most people think ‘natural’ = ‘safe’ and ‘I’ve been taking it for months’ = ‘it’s fine.’ But the enzyme flip-flop is real-and it’s silent. No warning signs until you’re bleeding out or your transplant gets rejected.
One thing I tell everyone: if your supplement has a ‘proprietary blend’ on the label, run. If it doesn’t list exact silymarin content, don’t touch it. And if you’re on anything with a narrow therapeutic window-ask your doctor *before* you open the bottle.
Also, if you’re reading this and you’re on cyclosporine? Just don’t. Seriously. I’m not joking. 🙏
Bailey Sheppard
I appreciate how balanced this is. I’ve been taking milk thistle for two years for mild fatty liver (no meds) and feel fine. But I also know people who’ve had bad reactions. It’s not black and white.
My advice? If you’re healthy and just using it for general support, go for a reputable brand with third-party testing. But if you’re on meds-especially blood thinners, seizure meds, or transplant drugs-don’t guess. Get tested. Talk to someone who knows pharmacology, not a YouTube influencer.
Also, side note: I’ve seen more people hurt by ‘detox teas’ and ‘liver cleanses’ than by milk thistle itself. The real problem isn’t the herb-it’s the narrative that your liver needs ‘cleansing.’ Your liver is already a 24/7 detox factory. You don’t need a supplement to help it. Just stop drinking soda and eat broccoli.
Still, this post is a public service. Thanks for writing it.
Girish Pai
Bro this is all just western medical dogma. In Ayurveda, milk thistle is called 'Katu' and it's been used for 5000 years with zero adverse events. CYP enzymes? Pfft. That’s just a reductionist model. Your body is not a machine. It’s a biofield. The interaction is not pharmacological-it’s energetic. The real issue is that allopathic medicine doesn’t understand prana.
Also, in India, we use milk thistle with guggul and turmeric and it’s synergistic. You westerners overcomplicate everything with your lab tests and percentages. Just drink the tea. Your liver will thank you. And if you’re on warfarin? Maybe you should stop taking that poison too.
Science is just one perspective. Tradition is wisdom. And we’ve been doing this longer than your FDA existed.
Kristi Joy
Thank you for sharing this so thoughtfully. I’m a nurse and I’ve had patients come in terrified because they started milk thistle and then their meds ‘stopped working.’ They didn’t know why. This post gives them the language to understand what’s happening-and the courage to talk to their doctor without feeling stupid.
One thing I always say: ‘Your body doesn’t know the difference between a pill and a plant.’ If it affects enzymes, it affects you. No judgment. Just awareness.
If you’re reading this and you’re unsure-ask your pharmacist. They’re not just the people who hand out pills. They’re your hidden safety net. And if you’re on warfarin? Please, please, please get your INR checked after 7 days. It’s a simple blood test. It could save your life.
You’re not alone. And you don’t have to figure this out alone.
Katelyn Sykes
My dad took milk thistle with his statin and got rhabdo. His CK was 18000. He’s fine now but he had to be hospitalized for a week. I never knew it could do that. I thought it was just a liver thing. This post saved me from making the same mistake. I’m getting my meds checked before I even buy a bottle. Thank you.
Also I bought the silybin-phosphatidylcholine one from Pure Encapsulations. No typos on the label. Worth the extra cash.
Yash Nair
INDIA HAS BEEN USING MILK THISTLE FOR CENTURIES AND NOBODY DIES. YOU AMERICANS ARE SO PARANOID ABOUT EVERYTHING. YOU THINK A PLANT CAN KILL YOU? HA. OUR GRANDMOTHERS USED IT WITH CURCUMIN AND THEY LIVED TO 100. YOUR DOCTORS ARE JUST TRYING TO SELL YOU MORE DRUGS. STOP BELIEVING THE WESTERN LIES.
IF YOU ARE ON WARFARIN THEN YOU ARE ALREADY DYING. MILK THISTLE IS JUST THE TRUTH TELLER. YOU SHOULD BE GRATEFUL IT SHOWED YOU YOUR MEDS ARE WEAK.
AND BY THE WAY THE FDA IS A CORRUPT ORGANIZATION. THEY TAKE MONEY FROM PFIZER. YOU THINK THEY WANT YOU TO KNOW THE TRUTH? LOL.



Write a comment