Psoriasis: What You Need to Know
Ever notice a red, scaly patch on your elbow or scalp that just won’t go away? Chances are you’re looking at psoriasis, a common skin condition that affects millions of people worldwide. It’s not just a cosmetic issue; the inflammation can be uncomfortable and sometimes linked to other health problems. The good news? You don’t have to live with endless flare‑ups. Understanding the basics helps you spot the signs early and take control.
Common Signs and Symptoms
Psoriasis shows up in a few recognizable ways. The most typical sign is thick, silvery patches that itch, burn, or crack. These plaques often appear on elbows, knees, scalp, lower back, and even nails. When nails get involved, you might see pitting, discoloration, or a crumbly surface. Some folks experience a sudden burst of spots – known as guttate psoriasis – after a strep throat infection.
It’s also worth noting that psoriasis can be sneaky. The patches may look mild at first, but they can get worse if you ignore them or expose the skin to triggers. If you notice any new, persistent rash, especially one that’s tender or bleeds, it’s time to see a dermatologist.
Managing Flare‑Ups and Treatment Options
Triggers vary from person to person, but a few common culprits show up again and again: stress, injury to the skin (like a cut or sunburn), certain medications, and smoking. Keeping a simple diary of your diet, stress levels, and skin changes can pinpoint what sparks your flare‑ups.
When it comes to treatment, there’s no one‑size‑fits‑all solution. Over‑the‑counter creams containing salicylic acid or coal tar can soften plaques and reduce redness. For tougher cases, prescription topicals (like corticosteroids or vitamin D analogues) work faster.
Phototherapy – controlled exposure to UV light – is another option that many dermatologists recommend. It can calm inflammation without daily creams. If psoriasis is widespread or stubborn, oral or injectable biologic drugs target the immune system directly and often bring rapid relief.
Don’t forget lifestyle tweaks. Moisturizing daily with fragrance‑free lotions keeps skin barrier strong, and gentle exfoliation helps remove dead skin cells. A balanced diet rich in omega‑3 fatty acids (found in fish, flaxseeds, and walnuts) may lessen inflammation for some people.
Finally, mental health matters. Because psoriasis can affect confidence, talking to a therapist or joining a support group can ease the emotional load. When your skin feels better, your mood usually follows.
Bottom line: psoriasis is manageable with the right mix of skin care, medication, and lifestyle choices. Keep an eye on your triggers, stay consistent with treatments, and don’t hesitate to ask a doctor for help when you need it. You deserve clear, comfortable skin – and with the tools above, you’re well on your way to getting it.
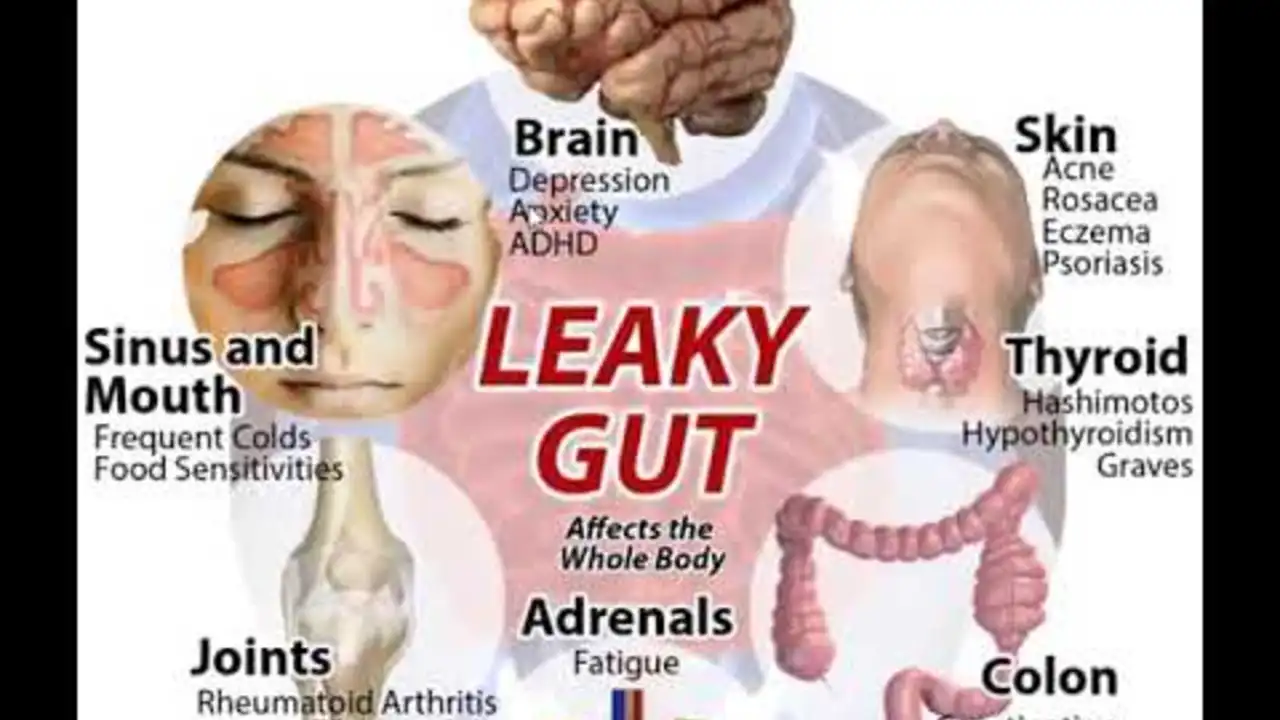
The Link Between Psoriasis and Gut Health: What the Research Says
As a blogger who's spent significant time delving into the realm of health and wellness, I've found a fascinating connection between gut health and psoriasis. Experts suggest that our gut health can potentially influence skin conditions like psoriasis, which we'll explore more in this post. We'll dive into the latest research, bringing to light the intricate relationship between our gut and skin. So, come along as we unravel this mind-boggling link, and aim to understand just how important our gut health can be.