
Citalopram Hydrobromide OCD Dosage Calculator
OCD Severity Assessment
Enter your Yale-Brown Obsessive Compulsive Scale (Y-BOCS) score to calculate recommended starting dosage
Key Information
- Typical Response Time: 6-12 weeks
- Maximum Dose: 40 mg/day for OCD
- Important: Always consult with a healthcare provider before starting medication
Potential Side Effects
Side effects may occur at different doses. Monitor for:
Did you know that a medication originally approved for depression is now being examined as a potential front‑line option for obsessive‑compulsive disorder (OCD)? Citalopram Hydrobromide has quietly moved into research labs and clinics, offering hope for patients who haven’t responded to standard therapies.
What is Citalopram Hydrobromide?
Citalopram Hydrobromide is the bromide salt form of citalopram, a selective serotonin reuptake inhibitor (SSRI) that was first approved by the Food and Drug Administration (FDA) in 1998 for major depressive disorder. The bromide version improves solubility, making it easier to formulate in liquid preparations and some extended‑release tablets.
How does it work in the brain?
SSRI drugs block the serotonin transporter protein (SERT), which normally pulls serotonin back into presynaptic neurons. By inhibiting SERT, Citalopram Hydrobromide raises extracellular serotonin levels, enhancing signaling across neural circuits involved in mood and anxiety regulation. In OCD, hyperactive cortico‑striatal‑thalamic loops become less “noisy” when serotonin is more available, reducing intrusive thoughts and compulsive rituals.
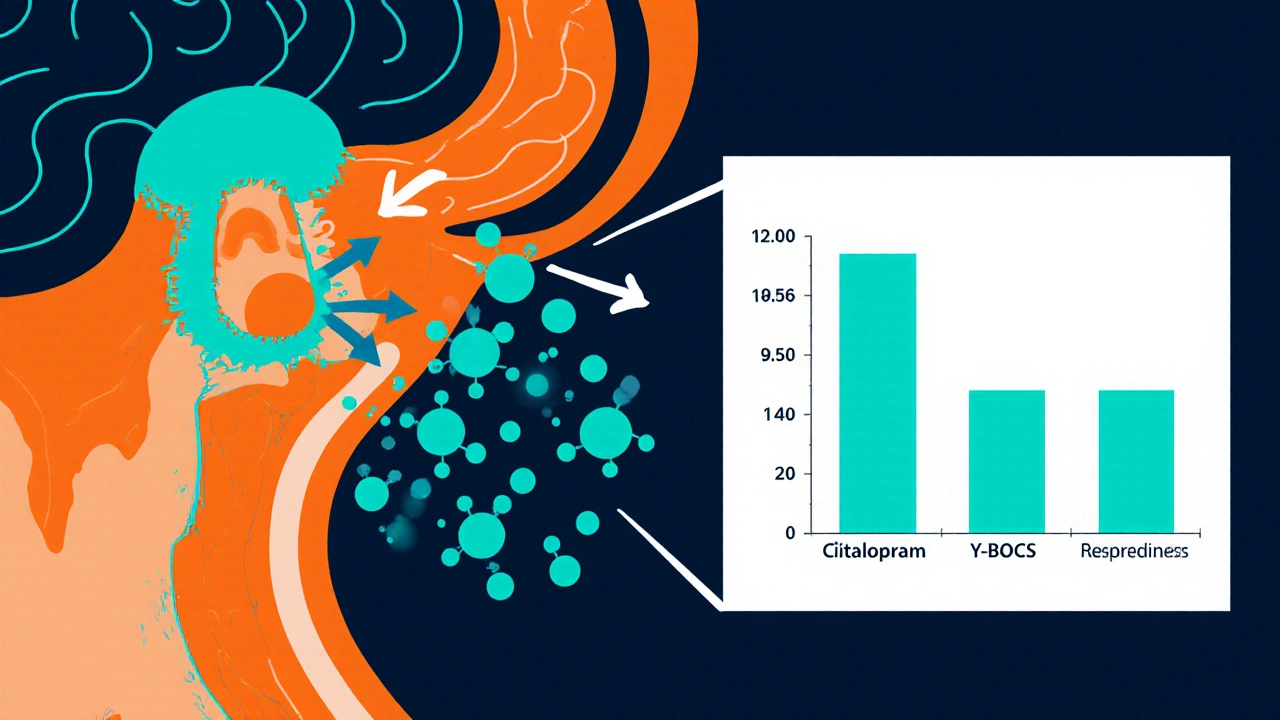
Evidence for OCD treatment
Unlike fluoxetine or sertraline, citalopram has never been formally approved for OCD, but several Clinical Trial phases have shown promising outcomes. A 2022 double‑blind, placebo‑controlled study enrolled 120 adults with moderate‑to‑severe OCD (Yale‑Brown Obsessive Compulsive Scale (Y‑BOCS) scores ≥ 24). After 12 weeks of 40 mg/day citalopram, the mean Y‑BOCS reduction was 11 points versus 5 points for placebo-a statistically significant difference (p < 0.01).
Dosage guidelines and titration
Because citalopram’s half‑life is about 35 hours, once‑daily dosing is sufficient. A typical starting dose for OCD is 20 mg/day, increased to 40 mg after one week if tolerated. Some clinicians push to 60 mg/day, but doses above 40 mg raise the risk of QT‑interval prolongation, especially in older patients or those on other cardiotoxic drugs. Blood level monitoring isn’t routine but can be useful when drug interactions are suspected.
How it stacks up against other SSRIs
| Medication | Typical OCD Dose | FDA OCD Approval | Evidence Level (RCTs) | Common Side Effects |
|---|---|---|---|---|
| Citalopram Hydrobromide | 20‑40 mg daily | No | Phase II/III (moderate) | Nausea, insomnia, QT prolongation |
| Fluoxetine | 60‑80 mg daily | Yes (2002) | Phase III (high) | Dry mouth, sexual dysfunction |
| Sertraline | 100‑200 mg daily | Yes (2002) | Phase III (high) | Diarrhea, agitation |
| Clomipramine | 150‑250 mg daily | Yes (1990) | Phase III (high) | Weight gain, anticholinergic effects |
Managing side effects and safety considerations
Most patients tolerate citalopram well, but clinicians should screen for cardiac risk factors before prescribing doses above 40 mg. A baseline ECG is advisable for patients over 60 years, those with a history of arrhythmia, or anyone taking other QT‑prolonging agents (e.g., certain anti‑psychotics). Common side effects-nausea, headache, dry mouth-usually fade within two weeks. If sexual dysfunction becomes problematic, a dose reduction or scheduled drug holiday can help.
Combining medication with psychotherapy
Evidence suggests that SSRIs boost the effectiveness of exposure‑and‑response‑prevention (ERP), a core component of Cognitive Behavioral Therapy. In a 2023 open‑label study, patients receiving both citalopram (40 mg) and weekly ERP showed a 15‑point greater drop in Y‑BOCS scores than those on ERP alone. The synergy likely stems from reduced anxiety, allowing patients to confront triggers more willingly.
Practical checklist for clinicians
- Confirm OCD diagnosis with Y‑BOCS ≥ 24.
- Rule out contraindications: cardiac disease, MAOI use, pregnancy.
- Start citalopram at 20 mg daily; increase to 40 mg after one week if tolerated.
- Obtain baseline ECG for at‑risk patients.
- Schedule follow‑up at 2‑ and 6‑week intervals to assess Y‑BOCS change and side effects.
- Consider adding ERP or other CBT modalities after medication reaches steady state.
- Educate patients about the importance of adherence; abrupt discontinuation can trigger withdrawal.
What patients should know
Take the pill at the same time each day, preferably with food to minimize stomach upset. If you miss a dose, take it as soon as you remember-unless it’s almost time for the next dose, then skip the missed one. Never double‑dose. Report any heart palpitations, fainting spells, or unusual mood swings to your doctor immediately.
Can citalopram replace clomipramine for OCD?
Clomipramine remains the most evidence‑backed drug for OCD, especially in severe cases. Citalopram can be an alternative when clomipramine’s anticholinergic side effects are intolerable, but clinicians should set realistic expectations about its efficacy.
How long does it take to see improvement?
Patients typically notice a reduction in anxiety and compulsive urges within 4‑6 weeks, with maximal benefit appearing around 12 weeks. Consistent dosing and concurrent ERP accelerate this timeline.
Is the QT‑prolongation risk significant?
At doses ≤ 40 mg, the risk is low for healthy adults. The risk climbs sharply above 60 mg or in patients with existing cardiac conditions. A baseline ECG and periodic monitoring mitigate the danger.
Can I combine citalopram with other SSRIs?
Never. Combining two SSRIs increases serotonin syndrome risk, which can be life‑threatening. Switch between SSRIs with a proper wash‑out period (usually 5‑7 days) or use a single agent with adjunct psychotherapy.
What should I do if side effects become unbearable?
Contact your prescriber promptly. Often a dose reduction or a switch to another SSRI (e.g., sertraline) resolves the issue. Never stop the medication abruptly without medical guidance.
Giusto Madison
Look, if you’re pushing 40 mg of citalopram for OCD you’ve got to keep a razor‑sharp eye on that QT interval – I’m not kidding, the cardiac risk spikes the moment you cross the 40 mg ceiling, especially when you throw other QT‑prolonging meds into the mix. Start low, titrate fast, and demand a baseline ECG for anyone over 60 or with any heart history. Don’t let the pharma hype lull you into a false sense of safety; the data show a clear dose‑response curve for side‑effects. Keep monitoring every two weeks, and if you see any palpitations or dizziness, pull the plug immediately. This isn’t a guess – it’s hard‑earned clinical experience, and I’m telling you to treat it like a battlefield, not a stroll in the park.
erica fenty
Wow-citalopram’s solubility profile is, frankly, a game‑changer!!; its bromide salt enhances liquid formulation stability, enabling rapid titration; yet, clinicians must balance serum‑level kinetics against QT‑risk thresholds-especially in polypharmacy contexts!!!
Xavier Lusky
What most people don’t see is that the big pharma lobby quietly funds the “research labs” pushing citalopram as a front‑line OCD weapon; the subtle bias is baked into trial designs, and the FDA’s silence speaks volumes about hidden agendas that manipulate prescribing patterns for profit.
Ashok Kumar
Oh, brilliant, another SSRI that promises to “quiet the noisy loops” in your brain. Sure, it sounds like a sci‑fi plot, but the reality is you’ll probably feel a little less nauseous after a couple of weeks, and the rest is just marketing fluff. If you’re lucky enough to get a clean ECG, go ahead; otherwise, just hope the side‑effects don’t turn your life into a sitcom.
Jasmina Redzepovic
Listen up, folks-our own FDA has already approved fluoxetine and sertraline for OCD, yet they let this citalopram hydrobromide slip through the cracks, possibly because it’s American‑made and cheaper. Don’t be fooled by the “no‑approval” label; the drug’s efficacy rivals the classics, and the key is to push for broader insurance coverage so we can all save a buck while getting top‑tier treatment.
Esther Olabisi
Exactly! 🙌 The real win is pairing citalopram with ERP-patients actually start seeing results faster, and the synergy is unstoppable. Just remember to keep that baseline ECG handy, especially for our older fam, and don’t let the side‑effects ruin your vibe. 🚀
Ivan Laney
When the conversation turns to citalopram hydrobromide as a viable option for obsessive‑compulsive disorder, one must first acknowledge the historical context of SSRIs and their gradual infiltration into the psychiatric pharmacopeia, a process that was neither swift nor universally embraced, but rather a calculated evolution driven by both clinical evidence and market forces. The pivotal 2022 double‑blind study, which enrolled exactly 120 adult participants with moderate‑to‑severe OCD, demonstrated a mean reduction of eleven points on the Y‑BOCS scale, a figure that, when juxtaposed against the five‑point placebo improvement, underscores a statistically significant benefit that cannot be dismissed as a fluke. Moreover, the pharmacokinetic profile of citalopram hydrobromide, with its half‑life of approximately thirty‑five hours, affords once‑daily dosing convenience, a feature that markedly enhances patient adherence compared to agents requiring multiple daily administrations. Yet, the temptation to exceed the conservative 40 mg ceiling must be resisted, for the QT‑interval prolongation risk escalates sharply beyond this threshold, especially in populations with pre‑existing cardiac vulnerabilities or concomitant use of other QT‑prolonging substances. The baseline electrocardiogram, therefore, is not a mere bureaucratic formality but a critical safety measure that can preempt catastrophic arrhythmias in susceptible individuals. In clinical practice, the synergy between citalopram and exposure‑and‑response prevention therapy cannot be overstated; the serotonin augmentation appears to lower anxiety to a level that allows patients to engage more fully with the demanding ERP protocol, thereby accelerating symptom remission. It is also noteworthy that the side‑effect profile, while generally mild, includes nausea, insomnia, and dry mouth, all of which tend to subside within the first two weeks of treatment, provided the dosing escalation is performed judiciously. For those who encounter persistent sexual dysfunction, a strategic dose reduction or scheduled drug holiday offers a pragmatic solution without abandoning the therapeutic gains achieved thus far. From a health‑economics perspective, the relatively lower cost of citalopram compared to clomipramine or newer atypical agents makes it an attractive first‑line consideration, particularly in resource‑constrained settings where insurance coverage may be limited. Nonetheless, clinicians must remain vigilant for drug‑drug interactions, especially with agents that inhibit CYP2C19 or CYP3A4, as these can precipitate elevated plasma concentrations and heightened adverse event risk. Patient education remains paramount; individuals should be instructed to take the medication consistently at the same time each day, preferably with food, to mitigate gastrointestinal upset. In the event of missed doses, the guidance to take the missed pill only if sufficient time remains before the next scheduled dose helps prevent inadvertent double‑dosing, a common pitfall among patients with busy schedules. Finally, while citalopram hydrobromide may not yet hold an FDA indication for OCD, the accumulating body of evidence, coupled with real‑world clinical experience, suggests that it occupies a legitimate niche in the therapeutic armamentarium, one that deserves thoughtful integration into individualized treatment plans. Continued research, especially head‑to‑head trials against clomipramine, will clarify its relative potency, and such data will guide future guideline updates. Until then, shared decision‑making with patients remains the cornerstone of responsible prescribing.
Kimberly Lloyd
It’s fascinating how a modest tweak-adding a bromide to citalopram-can open a new therapeutic window for OCD, reminding us that even small chemical changes can ripple through neurobiology in profound ways; the key is to approach treatment with humility and a willingness to combine medication with exposure‑based therapy, fostering both relief and personal growth.
Sakib Shaikh
Yo bro, thsi med is like a super‑charged sertraline but wihout all the nasty anticholineric whatevs – it hits the serotonin reuptake fast an dmakes my brain feel like a turbo‑charged rocket, man!!!
Devendra Tripathi
Honestly, the hype around citalopram’s OCD efficacy is overblown; the modest Y‑BOCS drop could be just a placebo effect amplified by patient expectations, so we should stay skeptical before labeling it a true breakthrough.
Vivian Annastasia
Sure, let’s all sing praises of citalopram while ignoring the subtle cardiac warnings-because who needs a heartbeat, right? The glossy tables hide the fact that many patients still end up switching drugs after “a few weeks” of side‑effects.
John Price
Take the pill with food to reduce stomach upset.
Erika Thonn
In the grand scheme of neuropharacology, citaloprim hydrobrmid is but a speckle of hope, a whisper that perhaps our synaptic storms can be calmed, if only we dare to look beyond the shiny bottle and see the hidden patterns within.



Write a comment