
Every year, tens of thousands of people in the U.S. get the wrong medication, the wrong dose, or a drug that clashes with something they’re already taking-all because a simple check was missed. And it’s not always the pharmacist’s fault. Sometimes, the error slips through because the patient didn’t ask the right questions or didn’t double-check what they were handed. You don’t need to be a doctor to help prevent these mistakes. You just need a simple, practical checklist you can use every time you pick up a prescription.
Why Your Pharmacy Visit Needs a Checklist
Pharmacies are busy. Pharmacists are overworked. Even the best ones can make a mistake. A 2023 study by the Institute of Medicine found that about 1 in 20 prescriptions filled in community pharmacies contain some kind of error-some minor, some life-threatening. Most of these errors happen during the final check before handing over the medication. That’s your moment to step in.You’re not supposed to be the pharmacist. But you are the one who takes the pills. You know your body, your allergies, your other meds, and your history better than anyone. If you don’t verify what you’re getting, no one else will.
Step 1: Bring Your Complete Medication List
Before you even walk into the pharmacy, make a list of everything you take. Not just prescriptions. Include over-the-counter pills, vitamins, supplements, and herbal remedies. Even if you think it’s harmless-like fish oil or melatonin-it can interact with your new medication.Write it down. Don’t rely on memory. Use your phone’s notes app, a printed sheet, or even a photo of your pill organizer. Bring it with you every time. Pharmacists are trained to check for interactions, but they won’t know about that turmeric supplement you take for joint pain unless you tell them.
Pro tip: Update this list every time you start or stop a medication. Keep it in your wallet or phone’s home screen so it’s always easy to find.
Step 2: Confirm Your Name and Date of Birth
This sounds basic, but it’s one of the most common causes of wrong-patient errors. Pharmacies often fill dozens of prescriptions in an hour. Names like Mary Johnson or David Lee are common. If the pharmacy staff doesn’t verify your identity, they might hand your prescription to someone else-or worse, give you someone else’s medicine.Don’t wait for them to ask. Say it first: “Hi, I’m John Rivera, born on March 14, 1982. I’m here for my blood pressure pill.”
Watch them check your ID against the label. If they don’t, ask: “Can you please confirm this is my prescription?”
Step 3: Check the Label Against Your List
When the pharmacist hands you the bottle, don’t just take it and leave. Stop. Look. Compare.On the label, check three things:
- Medication name-Is it exactly what’s on your list? (e.g., “Lisinopril” not “Lisinopril HCTZ” if you weren’t prescribed the combo.)
- Dose-Is it 10 mg or 20 mg? Did they accidentally double it?
- Directions-Does it say “take once daily” or “take twice daily”? If it says “take at bedtime” but you’ve always taken it in the morning, ask why.
If anything looks off-even if it’s just a little different-say something. Don’t assume it’s a typo. A wrong dose on a blood thinner or diabetes drug can land you in the hospital.
Step 4: Ask About New Medications
If this is a new prescription, don’t be shy. Ask the pharmacist:- “What is this for?”
- “What side effects should I watch for?”
- “Can I take this with my other meds?”
- “Do I need to avoid alcohol or certain foods?”
- “Is there a cheaper version?”
Most pharmacists are happy to explain. They’re trained to do this. And if they seem rushed or dismissive, that’s a red flag. You deserve clear answers.
One woman in Ohio noticed her new antidepressant had a different color than her last refill. She asked-and found out the pharmacy had accidentally given her a completely different drug. She caught it before taking one pill.

Step 5: Inspect the Pill Itself
If you’ve taken this medication before, you know what it looks like. Size. Shape. Color. Imprint. If it’s new, Google the pill using the imprint code (the letters or numbers on it) and the dose. Sites like Drugs.com or WebMD have pill identifiers.Don’t assume all pills with the same name look the same. Generic versions change manufacturers all the time. That doesn’t mean they’re wrong-but if it looks totally different from your last bottle and you didn’t get a notice, ask.
Example: Your usual metformin tablet is white and oval with “1000” on it. This time it’s a small blue round pill with “M52.” That’s not the same drug. It’s a different generic. Not necessarily dangerous-but you should know why it changed.
Step 6: Double-Check the Quantity and Refills
Count the pills if it’s a small bottle. If you were supposed to get 30 tablets and they gave you 60, ask why. Maybe it’s a mistake. Maybe it’s intentional-but you should know.Also check the refill info. Did they mark it as “0 refills” when you expected two? Did they accidentally remove a refill you’ve used before? Sometimes pharmacies change refill policies without telling you. If you’re out of refills and need more, you’ll find out too late if you don’t check.
Step 7: Take a Photo Before You Leave
This is simple, but powerful. Take a picture of the prescription label and the pills inside the bottle before you walk out. Store it in a folder on your phone called “Medications.”Why? If you get sick later, or if you need to see a new doctor, you’ll have proof of what you were actually given. If there’s a mix-up, you can show the photo to your doctor or pharmacist and say, “This is what I was given. This is what I was supposed to get.”
It’s not paranoia. It’s protection.
Step 8: Ask for a Medication Review
Many pharmacies offer free medication reviews-especially if you’re on five or more prescriptions. Ask: “Do you offer a medication review?”This is a 15- to 20-minute session where the pharmacist sits with you and goes over every pill you take. They’ll flag interactions, suggest changes, and help you organize your schedule. It’s free. It’s available. And most people don’t know about it.
Medicare Part D patients are even entitled to one per year. Ask your pharmacist or call your plan provider.

What If You Spot an Error?
If you catch a mistake-wrong drug, wrong dose, wrong name-don’t panic. Say: “I think there might be an error here.” Then show them your list and your photo. Most pharmacists will apologize and fix it right away.If they brush you off, ask to speak to the manager. If they still won’t fix it, call your doctor. And if you’re worried about your safety, go to another pharmacy. Your life is more important than loyalty to one location.
Make This a Habit
This checklist isn’t something you do once. It’s something you do every single time. Even if you’ve been getting the same pill for five years. Even if the pharmacist knows you by name. Even if you’re in a hurry.Medication errors don’t happen because pharmacists are careless. They happen because the system is fast, complex, and full of human pressure. You’re not being difficult. You’re being smart.
Keep this checklist on your phone. Print it out. Tape it to your fridge. Use it like a seatbelt. You don’t wear it because you expect to crash. You wear it because you know accidents can happen.
Final Tip: Talk to Your Doctor Too
Your pharmacist can catch errors at the counter. But your doctor controls what gets prescribed. Every six months, bring your medication list to your doctor. Say: “I’ve been taking all these. Are we still on the right plan?”Doctors change prescriptions all the time. Sometimes they forget to tell you. Or they write a refill without realizing you stopped the drug. A quick check-in prevents problems before they start.
Do I really need a checklist if my pharmacist is professional?
Yes. Even the most experienced pharmacists make mistakes. A 2022 study in JAMA Internal Medicine found that 18% of dispensing errors occurred in pharmacies with top safety ratings. Professionals are human. Systems fail. Your checklist isn’t a sign of distrust-it’s a backup plan.
Can I use this checklist for my elderly parents?
Absolutely. In fact, it’s even more important. Older adults often take 5-10 medications daily. They’re more likely to experience side effects and interactions. If your parent has memory issues, go with them. Bring the list. Ask the questions. Take the photo. You’re not overstepping-you’re saving their life.
What if I can’t read the label?
Ask the pharmacist to read it out loud to you. Or ask for a large-print label. Most pharmacies will do this for free. You can also use your phone’s camera to zoom in on the text. If you’re blind or have low vision, ask for a voice-labeled pill dispenser or a pharmacy that offers audio instructions.
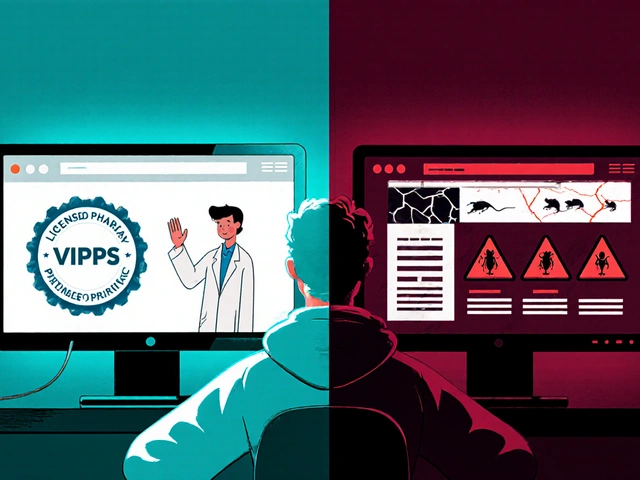
Is it okay to switch pharmacies to get better service?
Yes. If you feel rushed, ignored, or unsafe, switch. Your health is more important than convenience. Find a pharmacy that answers your questions patiently and lets you ask for a medication review. Many chain pharmacies offer this. Independent pharmacies often do it even better.
Can I use this checklist for over-the-counter drugs too?
Yes. Even aspirin, allergy pills, or sleep aids can interact with your prescriptions. If you’re on blood thinners, for example, taking ibuprofen can increase bleeding risk. Always check with your pharmacist-even for OTC drugs-especially if you’re on multiple medications.
Next Steps
Start today. Open your phone. Write down your current medications. Take a photo of your most recent prescription label. Print this checklist and stick it to your medicine cabinet. Next time you go to the pharmacy, use it. Don’t wait for something to go wrong. Prevent it before it happens.You don’t need a degree to keep yourself safe. You just need to care enough to ask.
Christian Landry
This is legit life-saving stuff 🙌 I always forget about the pill photo thing-just did it today after picking up my new statin. My phone’s now got a folder called ‘Meds That Don’t Kill Me’ 😅
Katie Harrison
I’ve been doing this for my mom since she turned 75... and I can’t believe how many times it’s caught errors. One time, they gave her a blood pressure pill that was twice the dose. She didn’t notice-thank god I did. This checklist? It’s not optional. It’s essential.
Michael Robinson
People think pharmacists are robots. They’re not. They’re tired. They’re human. And if you don’t check, no one will. It’s that simple.
Graham Abbas
I used to think this was paranoia... until my cousin ended up in ICU because they gave her a drug that interacted with her fish oil. She didn’t even know it was a supplement that mattered. This isn’t about distrust-it’s about survival. We live in a world where mistakes happen because no one wants to be the one to stop and ask. Don’t be that person.
Haley P Law
I JUST GOT A NEW PRESCRIPTION AND I USED THIS CHECKLIST. I SAW THE PILLS LOOKED DIFFERENT. I ASKED. THEY GAVE ME THE WRONG DRUG. I DIDN’T TAKE IT. I AM ALIVE BECAUSE OF THIS POST. I’M CRYING RIGHT NOW. THANK YOU.
Andrea DeWinter
If you’re helping an elderly parent or friend, do this with them. Don’t just hand them the list-walk them through it. Say ‘Let’s check this together.’ It’s not about control. It’s about care. And if they resist? Tell them you’re doing it because you love them. That usually works.
Steve Sullivan
I used to think asking questions made me annoying. Then I realized-no one else is gonna do it. So now I ask everything. What’s this for? Why this dose? Can I get it cheaper? And if they roll their eyes? I smile and say ‘Cool, thanks.’ Then I go to another pharmacy. My life’s worth the extra 10 minutes.
Evelyn Pastrana
Wow. So this is what happens when you stop treating healthcare like a game of telephone. I used to just grab my meds and run. Now I take pictures. I ask why. I even tell the pharmacist ‘I’m gonna Google this pill.’ They don’t mind. They’re just glad someone cares.
Arun Kumar Raut
In India, we don’t always have access to good pharmacies. But even here, this checklist works. My aunt took the wrong pills for a month because she didn’t check. She got sick. We learned. Now we do this every time. Simple. Smart. Necessary.
Carina M
While I appreciate the sentiment, I must point out that the term 'checklist' implies a mechanistic, procedural approach to a deeply personal and clinical process. One cannot reduce pharmaceutical safety to a bullet-pointed algorithm-this is an affront to the sanctity of the patient-provider relationship.
William Umstattd
I read this whole thing. It’s good. But honestly? If you’re that worried about your meds, why aren’t you seeing a specialist instead of relying on a pharmacy that’s understaffed and overworked? This is just a band-aid on a broken system.
Elliot Barrett
I don’t have time for this. I’ve got kids, a job, and a life. If I can’t trust the pharmacist, I shouldn’t be taking meds at all.



Write a comment