Coronary artery disease isn’t just a buzzword in doctor’s offices-it’s the number one killer worldwide. Every year, more than 18 million adults in the U.S. alone live with it, and it claims nearly 360,000 lives annually. Behind this statistic is a slow, silent process: fatty deposits clogging the very arteries that feed your heart. This isn’t just about cholesterol. It’s about inflammation, lifestyle, genetics, and how well your body handles stress over decades. If you’ve ever heard someone say, "He dropped dead out of nowhere," there’s a good chance coronary artery disease was the hidden cause.
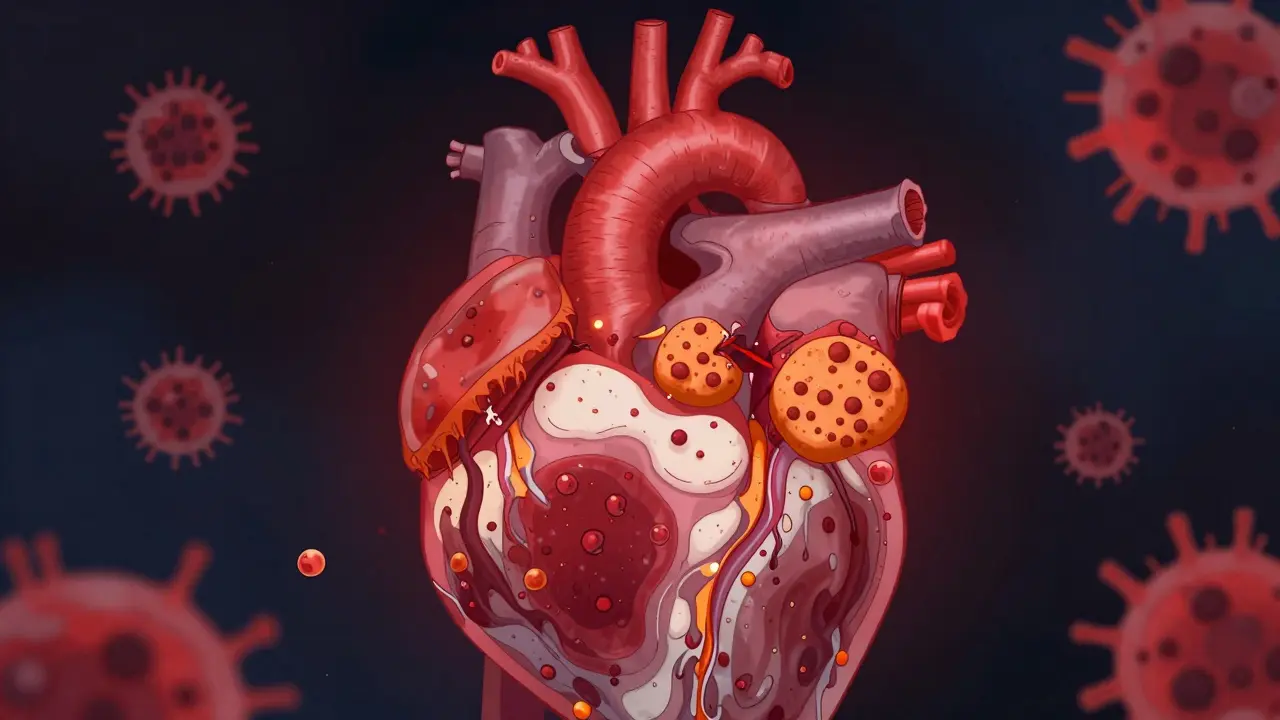
What Exactly Is Atherosclerosis?
Atherosclerosis is the root of coronary artery disease. It’s not a single event-it’s a decades-long buildup. Think of your arteries as pipes. Over time, instead of staying smooth and clear, they start accumulating gunk: cholesterol, calcium, cellular waste, and inflammatory cells. This gunk forms plaques inside the artery walls. These plaques don’t just grow bigger-they change in structure. Some become hard and stable. Others stay soft, with a big oily core and a thin outer shell. That’s the dangerous kind.
Stable plaques can narrow an artery by 70% or more, causing predictable chest pain when you exert yourself. But unstable plaques? They might only block 30-40% of the artery, yet they’re the ones that rupture. When they do, your body tries to seal the tear by forming a blood clot. That clot can completely block the artery, triggering a heart attack. That’s why so many people die suddenly-they never had warning signs.
The process starts with damage to the inner lining of the artery, often from high blood pressure, smoking, or high blood sugar. Once that lining is injured, LDL cholesterol (the "bad" kind) slips in and gets trapped. Immune cells rush in to clean it up, but they get overwhelmed. They turn into foam cells, which pile up and form the core of the plaque. Smooth muscle cells then build a fibrous cap over it. If that cap is thin, it’s like a balloon waiting to pop.
Who’s at Risk? The Real Culprits Behind CAD
Not everyone with high cholesterol gets heart disease. And not everyone who looks healthy is safe. Risk factors don’t just add up-they multiply. The latest guidelines from the American Heart Association and the American College of Cardiology break risk into three clear buckets: low, intermediate, and high.
Low risk? Less than 1% chance of a heart attack or cardiac death in a year. That’s rare. Most people fall into intermediate (1-3%) or high risk (over 3%). And here’s the scary part: 75% of all major heart events happen in the high-risk group.
So who’s in that high-risk group? People with:
- Diabetes (especially if it’s poorly controlled)
- History of heart attack, bypass surgery, or stents
- Heart failure, especially with preserved ejection fraction (HFpEF)
- Chronic kidney disease (eGFR below 60)
- Multiple blocked arteries (affecting more than one vascular bed)
- Smoking, even if they quit years ago
- High LDL cholesterol (above 190 mg/dL) or untreated high blood pressure
Obesity (BMI over 30) and physical inactivity aren’t just "bad habits"-they’re direct drivers of inflammation and insulin resistance, which accelerate plaque formation. Even if you’re not overweight, sitting all day increases your risk. And here’s something most people don’t realize: if you have atrial fibrillation, your risk of stroke and heart attack jumps significantly. That’s why doctors now treat CAD and AFib together, not as separate problems.
How Is It Diagnosed? Beyond the Chest Pain
Many people assume if you don’t have chest pain, you don’t have heart disease. That’s dangerous. About 30% of heart attacks happen without classic symptoms-especially in women, older adults, and people with diabetes. They might feel tired, nauseous, or have jaw pain instead.
Doctors use a mix of tools to find CAD before it’s too late:
- ECG (electrocardiogram): Checks your heart’s electrical rhythm. It can show signs of past damage or current stress.
- Stress tests: You walk on a treadmill or get medication to simulate exercise while your heart is monitored. If blood flow drops during stress, it points to blocked arteries.
- Coronary angiography: The gold standard. A thin tube is threaded into your artery, dye is injected, and X-rays show exactly where blockages are. It’s invasive, but it’s the only way to see the full picture.
- CT calcium score: A non-invasive scan that measures how much calcium is in your coronary arteries. More calcium = more plaque. A score above 100 means moderate risk; above 400 means high risk.
- Ankle-Brachial Index (ABI): Measures blood pressure in your ankle vs. arm. A low ratio suggests plaque in leg arteries-which often means it’s also in your heart arteries.
There’s also a growing category called INOCA-Ischemia with Non-Obstructive Coronary Arteries. These patients have heart pain and reduced blood flow, but no major blockages. Their problem might be tiny vessel disease, inflammation, or spasms. It’s harder to diagnose, but just as serious.

Treatment: It’s Not Just Pills and Surgery
Treating coronary artery disease isn’t about fixing one thing. It’s about changing your entire relationship with your body. The best outcomes come from combining three things: lifestyle, medication, and, when needed, procedures.
Lifestyle changes are the foundation. No pill replaces quitting smoking. No statin fixes a diet full of processed carbs and sugar. The Mediterranean diet-rich in olive oil, fish, nuts, vegetables, and whole grains-has been proven to reduce heart events by up to 30%. Regular movement matters too. Just 150 minutes a week of brisk walking cuts your risk significantly. You don’t need to run a marathon. Just move daily.
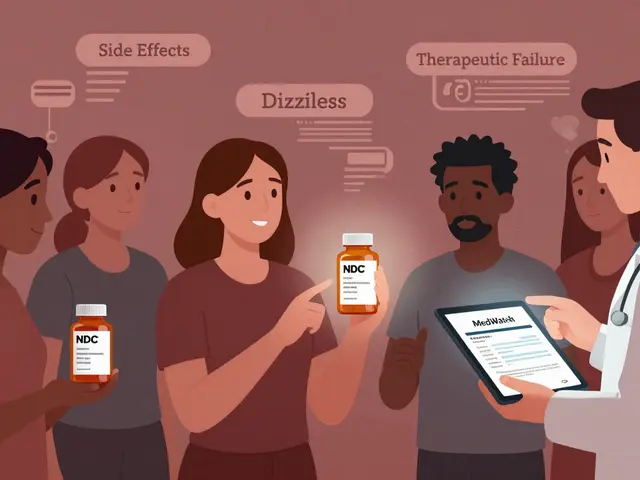
Medications are tailored to your risk level:
- Statins: Lower LDL cholesterol and stabilize plaques. Most people with CAD need them for life. High-intensity statins (like atorvastatin or rosuvastatin) are standard for high-risk patients.
- Antiplatelets: Aspirin or clopidogrel prevent clots. Used long-term after stents or heart attacks.
- ACE inhibitors or ARBs: Lower blood pressure and reduce strain on the heart, especially after a heart attack or if you have diabetes.
- Beta-blockers: Slow your heart rate and reduce oxygen demand. Often used after a heart attack.
- SGLT2 inhibitors and GLP-1 agonists: Originally for diabetes, these drugs now show strong heart protection-even in non-diabetics.
Some people need more than pills. If a major artery is blocked by more than 70%, doctors may recommend:
- Percutaneous Coronary Intervention (PCI): A balloon is inflated in the blocked artery, then a metal mesh stent is placed to keep it open. It’s minimally invasive and usually done the same day as diagnosis.
- Coronary Artery Bypass Grafting (CABG): Used when multiple arteries are blocked, especially if you have diabetes or heart failure. Surgeons take a vein or artery from another part of your body and create a detour around the blockage. Recovery takes weeks, but the results can last 15-20 years.
There’s no one-size-fits-all. A 55-year-old smoker with one blocked artery might do fine with a stent and lifestyle changes. A 70-year-old with diabetes, kidney disease, and three blocked arteries likely needs bypass surgery plus a full medical plan.
The New Frontiers: Personalized Care and Cardio-Oncology
The 2023 guidelines are a game-changer. They push doctors to stop treating CAD like a one-size-fits-all condition. Risk stratification isn’t just a checkbox-it’s the roadmap to your treatment. If you’re high risk, you need stronger meds, tighter monitoring, and faster action.
Another big shift is cardio-oncology. More people are surviving cancer. But chemotherapy and radiation can damage the heart. Now, cardiologists and oncologists work together from day one. If you’re getting cancer treatment and have CAD, your care team adjusts your heart meds to protect your heart without interfering with your cancer therapy.
Research is also focusing on plaque stabilization-not just removing blockages. New drugs are being tested to reduce inflammation in plaques, making them less likely to rupture. Some studies show that lowering LDL below 50 mg/dL can actually reverse plaque buildup over time. That’s something we didn’t believe possible 10 years ago.

What You Can Do Today
You don’t need to wait for symptoms. If you’re over 40, or have any risk factors, ask for a cholesterol panel, blood pressure check, and maybe a calcium score. Don’t ignore fatigue, shortness of breath, or unexplained discomfort. These aren’t just "getting older." They could be your heart asking for help.
Start small: swap soda for water. Walk 20 minutes after dinner. Get your blood pressure checked at least once a year. If you smoke, quit-no matter how long you’ve smoked. The damage starts healing within days.
Coronary artery disease isn’t a death sentence. It’s a signal. And with the right information and action, you can live a full, active life-even with plaque in your arteries.
Can you reverse coronary artery disease?
Yes, in many cases. While you can’t erase all plaque, aggressive treatment-like lowering LDL cholesterol below 50 mg/dL with high-intensity statins, combined with a heart-healthy diet and exercise-can shrink and stabilize plaques. Studies show this reduces the risk of heart attacks and strokes. It’s not about curing it completely, but making it less dangerous.
Is coronary artery disease hereditary?
Genetics play a role, but they’re not destiny. If a close relative had heart disease before age 55 (men) or 65 (women), your risk is higher. But lifestyle choices still control whether that genetic risk turns into actual disease. Two people with the same family history can have very different outcomes based on diet, activity, and smoking habits.
Do I need to take medication for life?
For most people with diagnosed CAD, yes. Medications like statins and antiplatelets aren’t just for symptoms-they prevent future events. Stopping them increases your risk of heart attack or stroke. Your doctor may adjust doses over time based on your progress, but stopping without medical advice is dangerous.
Can stress cause coronary artery disease?
Chronic stress doesn’t directly cause plaque buildup, but it contributes. It raises blood pressure, increases inflammation, and often leads to unhealthy habits like overeating, smoking, or skipping exercise. Stress also triggers heart rhythm problems and can cause coronary spasms. Managing stress through sleep, mindfulness, or therapy is part of heart disease prevention.
What’s the difference between a heart attack and angina?
Angina is chest pain or pressure that happens when your heart doesn’t get enough oxygen-usually during exercise or stress. It goes away with rest or nitroglycerin. A heart attack means a coronary artery is completely blocked, and heart muscle is dying. The pain doesn’t go away with rest. It’s often more severe, lasts longer, and may come with nausea, sweating, or shortness of breath. Angina warns you. A heart attack is an emergency.
Are stents better than bypass surgery?
It depends. Stents are less invasive and recovery is faster-usually a day or two. They’re ideal for single or double blockages. Bypass surgery is better for multiple blockages, especially if you have diabetes or heart failure. Bypass grafts last longer (15-20 years), while stents can re-narrow (restenosis) in about 5-10% of cases. Your doctor will choose based on your anatomy, age, and overall health.
What Comes Next?
If you’ve been diagnosed with CAD, your next step isn’t fear-it’s action. Schedule a follow-up with your cardiologist. Ask for your risk category. Ask what your LDL target should be. Ask if you need a calcium score or stress test. Don’t assume you’re fine because you feel okay.
If you haven’t been diagnosed but have risk factors, talk to your doctor about screening. Don’t wait for chest pain. Prevention isn’t optional-it’s the most powerful treatment we have.
Sue Stone
Been reading this while sipping my coffee. Honestly, I had no idea plaque could be so sneaky. I thought if you didn't have chest pain, you were fine. Guess I'm learning the hard way.
Janet King
Coronary artery disease is a chronic condition requiring lifelong management. Lifestyle modification remains the cornerstone of therapy, complemented by evidence-based pharmacologic intervention. Early detection through risk stratification significantly improves outcomes.
Stacy Thomes
STOP WAITING FOR SYMPTOMS!!! If you're over 40 and not checking your numbers, you're playing Russian roulette with your heart. I lost my dad at 52-he never had chest pain. Don't be him.
Dawson Taylor
The notion that atherosclerosis is merely a cholesterol issue is outdated. It is an inflammatory process, modulated by endothelial dysfunction, metabolic health, and systemic stress responses. The data supports this paradigm shift.
charley lopez
The calcium score is underutilized. It's non-invasive, cheap, and gives you a real-time snapshot of arterial burden. I got mine at 48-score of 320. Changed everything. No more denial.
Sallie Jane Barnes
I used to think statins were just for old people. Then my doctor said my LDL was 210 and my inflammation markers were through the roof. I started one. Lost 15 lbs, stopped feeling like a zombie. Best decision ever.
Susannah Green
Wait-so you're saying if I eat avocado every day and walk after dinner, I can actually reverse plaque?!?! I thought I was just doing this for my Instagram! I'm doing it for my heart now. #NoMoreDenial
Kerry Moore
This is one of the most comprehensive yet accessible summaries I’ve read on CAD. Thank you for clarifying the distinction between stable and unstable plaques-that’s critical for understanding sudden cardiac events.
Kerry Evans
Everyone talks about statins like they're magic pills. But let’s be real-most people on them still eat processed junk, sit all day, and blame genetics. You can’t medicate your way out of a life of neglect. The real problem isn’t cholesterol-it’s American culture.
Anna Pryde-Smith
They’re lying to you. The pharmaceutical industry doesn’t want you to know you can reverse this with diet alone. No pills. No stents. Just whole foods, fasting, and discipline. I did it. You can too. Stop trusting doctors who get paid by drug companies.
Oladeji Omobolaji
Back home in Nigeria, we don’t have statins or CT scans. My uncle had a heart attack at 50-he walked 10km to the clinic every day, ate yams and fish, stopped drinking palm wine. Lived 12 more years. Sometimes the old ways work better than the new gadgets.
Vanessa Barber
So… you’re telling me I don’t need to panic because I have a calcium score of 80? But I read somewhere that even 10 is bad? And isn’t LDL actually good if it’s large particles? And what about the sugar thing? I’m confused now.
dana torgersen
Okay so like… I’ve been reading this and I think maybe… like… the real issue isn’t the plaque… it’s the… uh… the emotional trauma? Like, chronic stress causes cortisol which causes inflammation which causes the… um… the… fatty stuff? I think? I’m not a doctor but I read a blog once…
Andrew Smirnykh
In Japan, they eat fish daily, walk everywhere, and have low CAD rates-even with high smoking rates. In the U.S., we treat symptoms instead of root causes. Maybe we need to look beyond pills and toward culture, community, and daily rhythm.



Write a comment