
Getting the right dose of medicine into your child isn’t just about following the label-it’s about staying alive. A single mistake in measurement can mean the difference between healing and hospitalization. For liquid medications, the most common errors aren’t caused by forgetfulness or bad intentions. They happen because parents use kitchen spoons, misread numbers, or assume a teaspoon is a teaspoon. The truth? A regular kitchen spoon can hold anywhere from 4 to 7 milliliters. The one your doctor prescribed? Exactly 5 mL. That’s not a small difference. It’s a tenfold risk of overdose if you confuse 0.5 mL with 5 mL.
Why Milliliters (mL) Are the Only Unit That Matters
Stop using teaspoons and tablespoons. Even if the label says "1 tsp," don’t trust it. The American Academy of Pediatrics, the CDC, and every major children’s hospital now agree: milliliters (mL) are the only safe unit for measuring children’s liquid medicine. Teaspoons and tablespoons vary by brand, country, and even how full you fill them. A 2020 study showed that using tools marked only in mL cut dosing errors by 42%. That’s not a suggestion-it’s a safety rule.
Look at your child’s prescription. If it says "5 mL," that’s the number you need. If it says "1 tsp," ask the pharmacist to rewrite it in mL. Many pharmacies still print both, even though the CDC’s PROTECT initiative has banned household units since 2010. Don’t wait for them to change. Demand mL-only instructions. Your child’s life depends on it.
The Right Tools for the Job
Not all measuring tools are created equal. Here’s what actually works:
- Oral syringes (1-10 mL): The gold standard. They’re accurate to the drop, easy to control, and perfect for doses under 5 mL. Studies show they’re 94% accurate. For babies and toddlers, they’re non-negotiable.
- Dosing cups (5-30 mL): Fine for older kids who can drink directly from the cup. But for doses under 5 mL, error rates jump to nearly 70%. They’re harder to read, spill easily, and kids often don’t finish them.
- Droppers (1-2 mL): Good for very small doses, like newborn antibiotics. But they’re hard to control. Use them only if the syringe doesn’t fit the bottle.
- Medication spoons: Only use if they’re labeled in mL and come with the medicine. Never use a regular kitchen spoon.
Here’s the hard truth: 7 in 10 parents use the wrong tool. If you’re using a spoon, cup, or eyedropper that didn’t come with the medicine, you’re playing Russian roulette with your child’s health.
How to Measure Accurately (Step by Step)
Even the best tool fails if you don’t use it right. Follow these steps every time:
- Shake the bottle if it says "shake well." Antibiotics and suspensions settle. If you don’t shake, your child gets less medicine-sometimes 30% less. That means the infection doesn’t clear.
- Use the right syringe. Always use the one that came with the medicine. Don’t swap it for a different one. Syringes aren’t interchangeable.
- Hold it upright. Place the syringe on a flat surface or hold it straight up. Don’t tilt it.
- Read the meniscus. Look at the liquid from eye level. The bottom of the curve (the meniscus) should line up with your dose mark. If you look from above or below, you’ll be off by a few drops.
- Give it slowly. Push the plunger gently into the side of your child’s mouth, near the cheek. Don’t squirt it in the front. That triggers the gag reflex. Kids spit it out. Aim for the cheek pouch.
- Check the dose twice. Read it. Then read it again. If it’s 2.5 mL, don’t guess. Count the lines. If you’re unsure, call the pharmacy.
Pro tip: Use a permanent marker to write the dose on the syringe if you give the same amount every day. Like "2.5 mL" next to the line. It saves time and prevents panic when you’re tired or stressed.

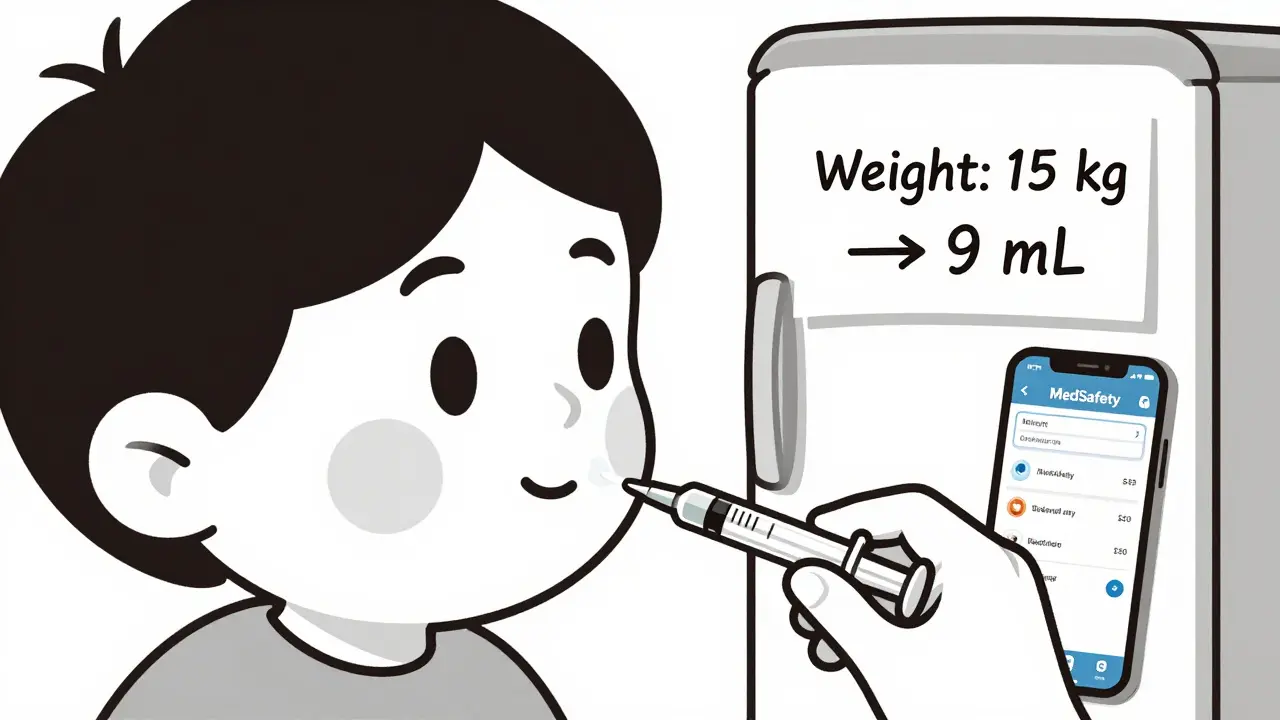
Weight-Based Dosing: What You Need to Know
Many children’s meds are dosed by weight-not age. That means you have to convert pounds to kilograms. The math is simple: divide pounds by 2.2.
Example: Your child weighs 33 pounds. 33 ÷ 2.2 = 15 kg. The prescription says 15 mg/kg/dose. So: 15 × 15 = 225 mg per dose. If the medicine is 125 mg per 5 mL, then 225 mg = 9 mL. That’s the dose.
If you’re not sure, don’t guess. Write down your child’s weight in kg and keep it on your fridge. Or use a free app like MedSafety (developed by Cincinnati Children’s Hospital) that does the math for you. Many parents don’t realize this step exists. That’s why so many overdoses happen-parents use age-based charts when the medicine requires weight.
What to Do When Your Child Refuses Medicine
Over 68% of parents say their child refuses medicine. It’s normal. But forcing it or mixing it into a full bottle of milk is dangerous. Here’s what works:
- Use a syringe to place the dose in the cheek pouch, not the tongue.
- Offer a small amount of apple sauce, yogurt, or juice right after. Don’t mix the medicine into it. You might not get the full dose.
- Try flavored versions. Many pharmacies can compound medicines with strawberry, grape, or bubblegum flavor.
- Let your child hold the syringe. Give them control. It reduces fear.
- Never use a bottle to give medicine. You can’t control how much they drink.
One parent in Sydney told me she kept her child’s favorite stuffed animal nearby during dosing. The child would only take medicine if the bear was "watching." It sounds silly-but it worked.
Common Mistakes (And How to Avoid Them)
These errors happen every day-and they’re preventable:
- Mixing up mg and mL: 5 mg is not 5 mL. One is a weight, one is a volume. Confusing them causes 36% of pediatric errors.
- Using old medicine: Antibiotics expire after 14 days once mixed. Throw them out. Don’t save them for next time.
- Sharing syringes: Never use the same syringe for multiple kids. Even if you rinse it. Bacteria can hide in the plunger.
- Not checking the concentration: Amoxicillin comes in 125 mg/5 mL, 250 mg/5 mL, and 400 mg/5 mL. If you give the wrong concentration, you overdose. Always read the bottle label.
- Assuming all pharmacies are the same: Only 57% of prescriptions include both mg and mL. Always ask for mL-only instructions.
What to Do If You Make a Mistake
If you gave too much, too little, or the wrong medicine:
- Call your pediatrician or poison control immediately. In Australia, call 13 11 26.
- Don’t wait for symptoms. Even if your child seems fine, errors can take hours to show up.
- Keep the medicine bottle and syringe. Bring them to the hospital.
- Write down what happened: time, dose, medicine name, tool used.
Most errors are caught before harm happens-if you act fast. Don’t feel guilty. Feel responsible. And next time, use a syringe.
What’s Changing in 2025
The FDA is pushing a new rule: all pediatric liquid medicines must come with a standard mL-only oral syringe. It’s expected to roll out fully by 2026. Some hospitals in Sydney already give out color-coded syringes (like NurtureShot) that match the medicine’s color. Red for antibiotics, blue for pain relief-so you can’t mix them up.
Smart dosing cups are coming too. Philips Healthcare is testing cups with built-in sensors that beep if you pour the wrong amount. They’re not on shelves yet, but they’re coming.
For now, the best tool is still the simple oral syringe. It costs less than $5. It’s reusable. It’s accurate. And it saves lives.
Can I use a kitchen teaspoon if I don’t have a syringe?
No. A kitchen teaspoon holds between 3.9 and 7.3 mL-not the standard 5 mL. That’s a 20% to 200% error. For a child, that could mean an overdose or under-dose. Always use the syringe that came with the medicine or buy a new one from the pharmacy. They’re cheap and lifesaving.
What if my child spits out the medicine?
Don’t give another full dose. Wait until the next scheduled time. Giving extra medicine can cause overdose. If your child spits out more than half, call your doctor. They may adjust the next dose. Always aim the syringe toward the cheek, not the front of the mouth, to reduce spitting.
How do I know if the medicine is the right strength?
Check the label for concentration: it will say something like "125 mg per 5 mL." Never assume all amoxicillin or ibuprofen is the same. Different brands have different strengths. If the label doesn’t show mL, ask the pharmacist to rewrite it. Write it down on the bottle with a marker.
Should I use a dosing cup for my 5-year-old?
Only if the dose is 5 mL or more. For doses under 5 mL, use an oral syringe. Dosing cups are harder to read accurately for small amounts, and kids often don’t drink all of it. Syringes are more precise and reliable, even for older children.
Is it safe to mix medicine with milk or juice?
Only if your doctor or pharmacist says it’s okay. Some medicines lose strength when mixed. If you do mix it, use a small amount-just enough to mask the taste. Give the whole thing right away. Don’t save the rest. Your child might not finish it, and you won’t know if they got the full dose.
What should I do if I’m not sure about the dose?
Call your pharmacy or pediatrician. Don’t guess. Don’t rely on memory. Don’t ask online. Every child is different, and even small errors can be dangerous. Pharmacists are trained to help with dosing. Use them. It’s what they’re there for.
Bennett Ryynanen
Bro seriously? I used a kitchen spoon last week and my kid didn’t die. Chill the fuck out. You sound like a CDC ad on loop.
Deepika D
Let me tell you something - I’m a pediatric nurse in Delhi, and I’ve seen too many kids brought in because mom used a soup spoon because ‘it’s close enough.’ No, it’s not. A teaspoon isn’t a teaspoon. Not in India, not in the US, not anywhere. I keep oral syringes in my bag at all times. I give them out for free to families who can’t afford them. You don’t need to be rich to save your child’s life - you just need to stop guessing. Buy a $3 syringe. Shake the bottle. Read the meniscus. Write the dose on it with a marker. Do it every time. Even when you’re exhausted. Even when your baby is screaming. Even when you’re up for the third night in a row. That syringe? It’s your shield. And your child deserves that shield. No excuses. Not anymore.
Darren Pearson
While the sentiment behind this post is commendable, one must acknowledge the structural inequities that prevent many caregivers from accessing standardized dosing tools. The assumption that all parents can readily procure oral syringes is a privilege-laden fallacy. Moreover, the demonization of household utensils ignores cultural and socioeconomic contexts in which pharmaceutical infrastructure is under-resourced. A more nuanced discourse would advocate for policy-level interventions rather than individualized behavioral mandates.
Jenny Salmingo
I just started using the syringe after reading this. My son used to spit everything out. Now I aim for the cheek and he doesn’t even flinch. Small change. Big difference. Thank you.
anggit marga
Why do Americans always act like they invented medicine? We use spoons in Nigeria and our kids grow up fine. You people overthink everything
Stewart Smith
So let me get this straight… you’re telling me the only reason my kid didn’t die from my sloppy dosing is because I got lucky? Wow. Thanks for the guilt trip, Dr. CDC.
Retha Dungga
Life is chaos anyway why fight the dose 🌌💊
Aaron Bales
Use the syringe. Always. No exceptions. Done.
Branden Temew
If we’re going to quantify every drop of medicine, why not quantify the emotional trauma of parenting under constant fear? Are we measuring doses… or are we measuring our own helplessness?
Frank SSS
Look I’m not saying the syringe thing isn’t good… but I’ve given my kid meds with a dropper for three years and he’s still alive. Also, the pharmacist gave me the wrong concentration once and I didn’t even notice until the bottle was empty. So yeah… I’m basically a walking medical error. But hey, I still love my kid. That counts for something right? 😅
Paul Huppert
Just bought the syringe today. Took me 3 tries to get the dose right. Felt like a scientist. My kid looked at me like I was weird. Worth it.
Hanna Spittel
Did you know the FDA is working with Big Pharma to make you buy syringes so they can charge you more? 🤔 They’ve been pushing this for years… and now you’re all drinking the Kool-Aid. 😏
Urvi Patel
Why are you so obsessed with mL nobody cares about your precision culture you just want to feel superior
Chandreson Chandreas
My daughter used to cry every time I gave her medicine… until I started letting her hold the syringe. Now she says ‘my turn’ and giggles. 🤖💙
Turns out control beats coercion. Who knew? Also… the marker trick? Genius. I wrote ‘2.5’ on mine last week. Still there. Still saving us. 🙏





Write a comment