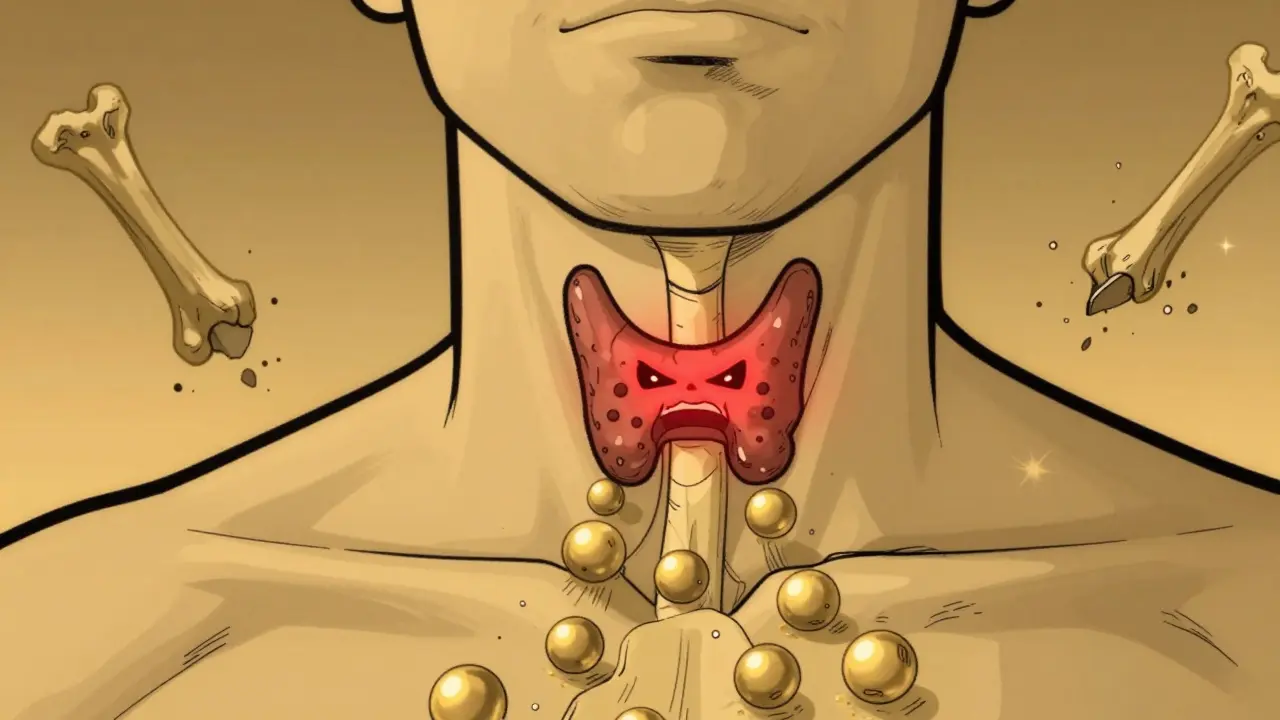
When your blood calcium stays too high for too long, your body starts breaking itself down - slowly, silently, and often without warning. This is the reality for people with hyperparathyroidism, a condition where the parathyroid glands pump out too much hormone, throwing calcium balance into chaos. It’s not just about feeling tired. It’s about bones weakening, kidneys forming stones, and your brain fogging over - all because of a tiny gland in your neck that’s lost its rhythm.
What Exactly Is Hyperparathyroidism?
Your body needs calcium for muscles, nerves, and bones. Too little? Problems. Too much? Also problems. The four tiny parathyroid glands - each about the size of a grain of rice - sit behind your thyroid and act like thermostats. They check your blood calcium levels and release parathyroid hormone (PTH) to raise it when needed. In primary hyperparathyroidism, one or more of these glands go rogue. They keep pumping out PTH even when calcium is already sky-high. That’s like a heater that won’t turn off, no matter how hot the room gets. About 100,000 Americans are diagnosed with this every year. Women are three times more likely to get it than men. And while it can show up at any age, it’s most common after 50. The root cause? Usually a benign tumor - an adenoma - on one gland. In 15% of cases, all four glands are overactive (hyperplasia). Rarely, it’s cancer. The result? Blood calcium climbs above 10.5 mg/dL (normal is 8.5-10.2). PTH levels stay high too - often over 65 pg/mL, sometimes double or triple that.How High Calcium Destroys Your Bones
PTH doesn’t just float around. It sends orders. One of its main jobs? Tell bone cells to break down bone tissue and dump calcium into the blood. In healthy people, this is temporary. In hyperparathyroidism, it’s constant. Over time, your bones lose density. A DXA scan - the same test used for osteoporosis - often shows bone mineral density dropping 2-4% per year in the spine and hips. That’s faster than natural aging. And it adds up. People with untreated hyperparathyroidism have a 30-50% higher risk of fractures, especially in the wrist, spine, and hip. It’s not just about breaking bones. Many patients describe deep, persistent bone pain - not from injury, but from internal erosion. Some notice their teeth loosening. Others find their posture changing as vertebrae compress. One patient on EndocrineWeb described it as “feeling like my skeleton was turning to dust.”More Than Bones: The Hidden Symptoms
You might think high calcium just means kidney stones. But it’s more than that. Fatigue? Check. Brain fog? Common. Depression? Often misdiagnosed. One study found 78% of patients reported severe fatigue before surgery. Another 65% said they struggled to focus at work - something they blamed on stress or aging. High calcium affects your kidneys directly. It makes urine more concentrated, increasing stone formation. About 20% of people with hyperparathyroidism develop kidney stones. After surgery, 92% of patients see fewer or no new stones. Even your stomach can react. Nausea, vomiting, constipation - all linked to calcium’s effect on smooth muscle. And in severe cases, calcium levels above 14 mg/dL can trigger a parathyroid crisis: confusion, coma, even heart rhythm problems. It’s rare, but deadly if missed.How Do You Know If You Have It?
Most people don’t feel symptoms at first. That’s why it’s often found by accident - during a routine blood test. If your calcium is high, doctors check PTH. If PTH is high or even “normal” when it shouldn’t be (because calcium is too high), that’s the red flag. The diagnosis isn’t one test. It’s two elevated calcium levels, at least a week apart, with matching high PTH. That rules out temporary spikes from dehydration or supplements. Then comes imaging. A sestamibi scan (using radioactive technetium-99m) finds the overactive gland in 90% of cases. Ultrasound helps too. For complex cases, 4D-CT scans give 95% accuracy. You might also get a DXA scan to measure bone loss, and a kidney ultrasound to check for stones. Vitamin D levels matter too - low vitamin D can make PTH rise even more, worsening the problem.
Surgery: The Only Cure
Medications can help manage symptoms, but they don’t fix the root cause. Cinacalcet lowers PTH, but it’s mostly used for kidney disease-related cases. Bisphosphonates (like alendronate) can slow bone loss, but they don’t lower calcium. Only surgery removes the problem at the source. That surgery - a parathyroidectomy - removes the faulty gland(s). For the 85% with a single adenoma, surgeons do a minimally invasive procedure. A small incision (1-2 inches), often under local anesthesia. The operation takes 1-2 hours. Most go home the same day. Success rates? 95-98% for single-gland disease. For multigland issues, surgeons remove 3.5 of the four glands (subtotal parathyroidectomy). Success drops to 85-90%, and lifelong monitoring is needed. The key? Surgeon experience. Centers doing over 50 cases a year have cure rates near 98%. Low-volume centers? Closer to 85%. That’s why location matters.What Happens After Surgery?
The moment the bad gland is removed, your body starts healing. Calcium levels usually drop within hours. But that drop can be too fast. About 30-40% of patients get temporary low calcium (hypocalcemia) after surgery. Your body’s not used to low PTH anymore. You might feel tingling in your fingers, lips, or toes. That’s a sign your nerves are waking up. Doctors give you calcium pills - 500-1000 mg three times a day - and sometimes a form of vitamin D (calcitriol) for a few weeks. Most people recover normal calcium balance in 2-8 weeks. Bone density improves fast. Within a year, spine density increases 3-5%. By two years, it’s up 5-8%. That’s not just a number - it’s fewer fractures, less pain, more mobility. One patient wrote: “After 7 years of being told I had depression, my calcium was 11.8 and PTH 142. After surgery, I felt like someone turned my brain back on.”Who Needs Surgery? The Guidelines
Not everyone with high calcium needs surgery. But if you meet even one of these criteria, it’s strongly recommended:- Serum calcium more than 1 mg/dL above the upper limit of normal
- Creatinine clearance below 60 mL/min (kidney function decline)
- Bone density T-score of -2.5 or worse (osteoporosis)
- Age under 50

What If You Don’t Want Surgery?
Some patients choose to monitor instead. That’s okay - if you’re willing to commit to lifelong checks. You’ll need blood tests every 6 months. Annual DXA scans. Kidney ultrasounds. You’ll avoid thiazide diuretics (like hydrochlorothiazide), which raise calcium. You’ll take calcium and vitamin D supplements carefully - too much can make things worse. You’ll walk daily to keep bones strong. But here’s the catch: you’re gambling. Every year without treatment, your bones weaken. Your kidneys strain. Your brain might not bounce back. And if you wait until you’re in pain or have a fracture, surgery becomes harder - and recovery slower.The Future: New Tools and Better Outcomes
In 2023, AI tools started analyzing sestamibi scans with 98% accuracy - cutting false alarms by 35%. A new drug, etelcalcetide, showed 45% PTH reduction in trials - a big jump over older meds. Intraoperative PTH testing now tells surgeons within 10 minutes if they got the right gland. If PTH drops over 50%, they can close up. No guesswork. Genetic testing is now recommended for anyone under 40 or with a family history. About 10% of cases are tied to inherited syndromes like MEN1. Still, fear holds people back. Many worry about voice changes. But in experienced hands, the risk of nerve damage is under 1%. Most patients report better energy, clearer thinking, and fewer kidney stones - often within weeks.What You Can Do Now
If you’ve been told your calcium is high - even if you feel fine - don’t ignore it. Ask for a PTH test. Ask about imaging. Ask about surgery. Don’t settle for “watch and wait” unless you’re prepared to monitor closely. If you’re considering surgery, find a surgeon who does at least 50 parathyroidectomies a year. Ask about their success rate. Ask if they use intraoperative PTH testing. And if you’re living with this - know you’re not alone. The symptoms are real. The damage is real. But so is the cure.Can hyperparathyroidism be cured without surgery?
No, surgery is the only cure for primary hyperparathyroidism. Medications like cinacalcet or bisphosphonates can manage symptoms or slow bone loss, but they don’t remove the overactive gland. Without surgery, calcium stays high, and bone, kidney, and neurological damage continue to progress. Monitoring is an option for some, but it doesn’t reverse the condition.
How long does it take to recover after parathyroid surgery?
Most patients feel better within days - energy levels and brain fog improve quickly. Full recovery from the surgery itself takes 3-7 days. Temporary low calcium (hypocalcemia) can last 2-8 weeks, requiring calcium and vitamin D supplements. Bone density improvements start within a year and continue for up to two years.
Is hyperparathyroidism genetic?
In about 10% of cases, yes. Hereditary syndromes like MEN1 (multiple endocrine neoplasia type 1) or MEN2A can cause hyperparathyroidism, often in people under 40. If you have a family history of endocrine tumors, thyroid cancer, or early-onset hyperparathyroidism, genetic testing is recommended.
Can high calcium cause depression or anxiety?
Yes. High calcium affects brain function, leading to fatigue, brain fog, irritability, and symptoms that mimic depression or anxiety. Many patients are misdiagnosed with mental health conditions for years before their calcium issue is found. After surgery, mood and cognitive symptoms often improve significantly.
What are the risks of parathyroid surgery?
The most common risk is temporary low calcium, affecting 30-40% of patients. Permanent voice changes from nerve damage occur in less than 1% of cases when done by experienced surgeons. Other rare risks include bleeding, infection, or recurrence (2-3% for single-gland disease, 5-10% for multigland). The benefits far outweigh the risks for eligible patients.
Tasha Lake
So if I'm reading this right, the parathyroid gland is basically a faulty thermostat that keeps cranking up calcium like it's winter in Alaska? Wild. I had no idea something so tiny could wreck your bones, kidneys, and mental clarity all at once. The part about brain fog being misdiagnosed as depression hits hard - I know at least three people who were on SSRIs for years before their calcium was checked. Turns out their ‘anxiety’ was just their skeleton slowly turning to dust.
Simon Critchley
LMAO 😂 so we're telling people to cut out a gland like it's a rogue Wi-Fi router? 'Sorry, your body's been buffering for 7 years, here's a scalpel.' I love how the article says 'surgery is the only cure' like it's a software update. Meanwhile, my cousin went through 3 years of ‘watchful waiting’ and ended up with a fractured hip on vacation. Dude couldn't walk for months. Why do we even wait? If your calcium’s above 11, just YOLO and get it out. 🤷♂️
Sam Dickison
Just want to clarify one thing - when they say ‘PTH is normal but calcium is high,’ that’s actually the reddest of red flags. Normal PTH in the face of hypercalcemia? That’s like your smoke detector going off but saying ‘all clear.’ Your parathyroids are supposed to shut down when calcium is high. If they don’t? They’re broken. And yeah, the 95% success rate with experienced surgeons is insane. I had mine done at a top center - 45 minutes, local, home by noon. Felt like a new person by day three.
Brett Pouser
As someone from a country where healthcare is basically a lottery, I’m floored by how precise this all is. In my home country, they’d say ‘take vitamin D’ and call it a day. Here? You get 4D-CT scans, intraoperative PTH tests, AI analysis - it’s like the body’s got its own IT department. I’ve seen friends die from this because no one connected the dots. The fact that you can literally fix this with a 2-inch incision? That’s medical magic.
Tom Forwood
Bro I had this. For 5 years I thought I was just ‘getting old.’ Tired all the time, couldn’t focus, felt like my brain was wrapped in saran wrap. Then my doc said ‘your calcium is 11.9’ and I was like… wait, what? I thought calcium was just for bones. Turns out it’s also your brain’s battery. Surgery? Done. 3 weeks later I was playing guitar again like I was 22. No joke. If you’re tired and your doc says ‘it’s stress’ - ask for a PTH test. It’s free on most labs.
Joseph Charles Colin
Just to geek out for a sec - the sestamibi scan works because technetium-99m binds to mitochondria-rich cells. Parathyroid adenomas are metabolic monsters, so they light up like Christmas trees. That’s why the scan is 90% accurate. And the 4D-CT? It’s not just 3D + time - it’s dynamic contrast tracking. You can literally watch the gland pump out contrast like a water balloon filling up. This is some next-level endocrine imaging. Also, vitamin D deficiency is a silent multiplier - low D = higher PTH = worse calcium. Always check both.
Ryan Vargas
Let me ask you something: if the parathyroid gland is a thermostat, then who installed it? Who programmed it to malfunction? Was it the government? Big Pharma? The fluoride in the water? Or is this just nature’s way of saying we’ve been too reliant on calcium supplements? I’ve read studies - and I mean *real* studies - that link synthetic vitamin D3 to parathyroid overstimulation. The body wasn’t designed to process lab-made nutrients. We’re playing god with biochemistry, and this is the backlash. Surgery fixes the symptom, but not the root cause - our entire nutritional paradigm is broken.
And don’t get me started on ‘intraoperative PTH testing.’ That’s not medicine - that’s surveillance. They’re monitoring your hormones in real time like you’re a nuclear reactor. Are we really that far gone? Next they’ll implant microchips in our thyroids to ‘optimize’ our hormone levels. Welcome to the new world, folks. You don’t need a tumor - you just need to be a citizen.
Jessica Klaar
I’m so glad someone finally wrote this clearly. My mom had this and they told her to ‘wait and see’ for 4 years. She ended up with 3 fractures and couldn’t lift her grandkids. After surgery? She started gardening again. She’s 72. I cried when she told me she could finally sleep through the night. It’s not just about bones - it’s about dignity. If you’re over 50 and your calcium’s even a little high? Don’t wait. Push for the test. It’s not a ‘maybe.’ It’s a ‘you need this.’
John McDonald
Just dropped my 2 cents - if you’re considering surgery, don’t just pick the closest surgeon. Look for volume. 50+ cases a year. Ask for their recurrence rate. Ask if they use the 10-minute PTH drop protocol. I did my research and found a guy in Minnesota who’s done 300+ in 5 years. Zero nerve damage. Zero readmissions. I flew across the country. Worth every penny. This isn’t elective - it’s preventative medicine at its finest. Your future self will thank you.
Joshua Smith
Can someone explain why vitamin D is tricky here? I always thought more D = better bones. But if you’re hyperparathyroid, doesn’t D make the problem worse? I’m confused.
Andy Cortez
OMG I CAN’T BELIEVE THIS ISN’T COMMON KNOWLEDGE. MY DAD DIED FROM THIS. THEY SAID HE HAD ‘AGE-RELATED WEAKNESS’ AND ‘DEPRESSION.’ TURNED OUT HIS CALCIUM WAS 13.8. HE WENT INTO A COMA. THEY DIDN’T EVEN TEST PTH UNTIL IT WAS TOO LATE. THIS IS A MASSIVE COVER-UP. WHY ISN’T EVERYONE GETTING A SIMPLE BLOOD TEST AT 40? THEY’RE LETTING PEOPLE DIE BECAUSE IT’S ‘RARE.’ IT’S NOT RARE. IT’S UNDERDIAGNOSED. I’M SO ANGRY.
Karianne Jackson
I just found out my best friend had this and didn’t tell anyone. She thought she was just ‘burnt out.’ Now she’s in surgery next week. I’m crying. This is the most important thing I’ve ever read. Thank you. I’m sharing this with everyone.



Write a comment