
Psoriasis Diet Checker
Recommended Foods for Psoriasis
Fatty Fish
Rich in omega-3s (EPA & DHA) that reduce inflammation.
Leafy Greens
Loaded with antioxidants like lutein to fight oxidative stress.
Berries
High in vitamin C and polyphenols for skin protection.
Nuts & Seeds
Plant-based omega-3s and fiber to support gut health.
Olive Oil
Extra-virgin contains oleocanthal, a natural anti-inflammatory.
Probiotic Foods
Support gut-skin axis for better immune regulation.
Common Triggers to Avoid
Processed Sugar
Spikes insulin and increases inflammatory cytokines.
Refined Carbs
Cause blood sugar spikes linked to inflammation.
Saturated Fats
Raise LDL cholesterol and worsen skin scaling.
Gluten
May trigger autoimmune responses in sensitive individuals.
Nightshades
Contain solanine, which may irritate skin in some people.
Alcohol
Increases inflammation and can worsen symptoms.
Quick Takeaways
- Focus on anti‑inflammatory foods like fatty fish, leafy greens, and nuts.
- Avoid processed sugars, excess saturated fats, and common triggers such as gluten and nightshades.
- Boost gut health with probiotic‑rich yogurts, kefir, and fermented veggies.
- VitaminD and omega‑3s have the strongest evidence for soothing flare‑ups.
- Simple meal‑planning tips keep you on track without feeling restricted.
When you hear the word "diet," you might picture strict calorie counting or trendy smoothies. Psoriasis is a chronic autoimmune skin condition that causes red, scaly patches, and it’s surprisingly sensitive to what lands on your plate. Research from dermatology clinics in Australia and the US shows that an psoriasis diet rich in anti‑inflammatory nutrients can reduce itching, soften plaques, and even cut down on medication dosage for some people. Below is a no‑fluff playbook that tells you exactly which foods to load up on, which ones to keep out of the pantry, and how to turn the advice into everyday meals.
Why Food Matters for Psoriasis
Psoriasis isn’t just a skin problem; it’s a systemic inflammatory disorder. When you eat foods high in refined sugar or saturated fat, your body releases cytokines-chemical messengers that fan the inflammatory fire. Over time, that fire can manifest as larger or more frequent skin lesions. Conversely, nutrients like omega‑3 fatty acids, antioxidants, and vitaminD act as natural fire‑breakers, calming the immune system and supporting skin cell turnover.
Three scientific pillars back this link:
- Omega-3 fatty acids lower prostaglandin production, which reduces plaque thickness.
- Antioxidants neutralize oxidative stress that can trigger flare‑ups.
- Vitamin D modulates T‑cell activity, a key driver in psoriasis.
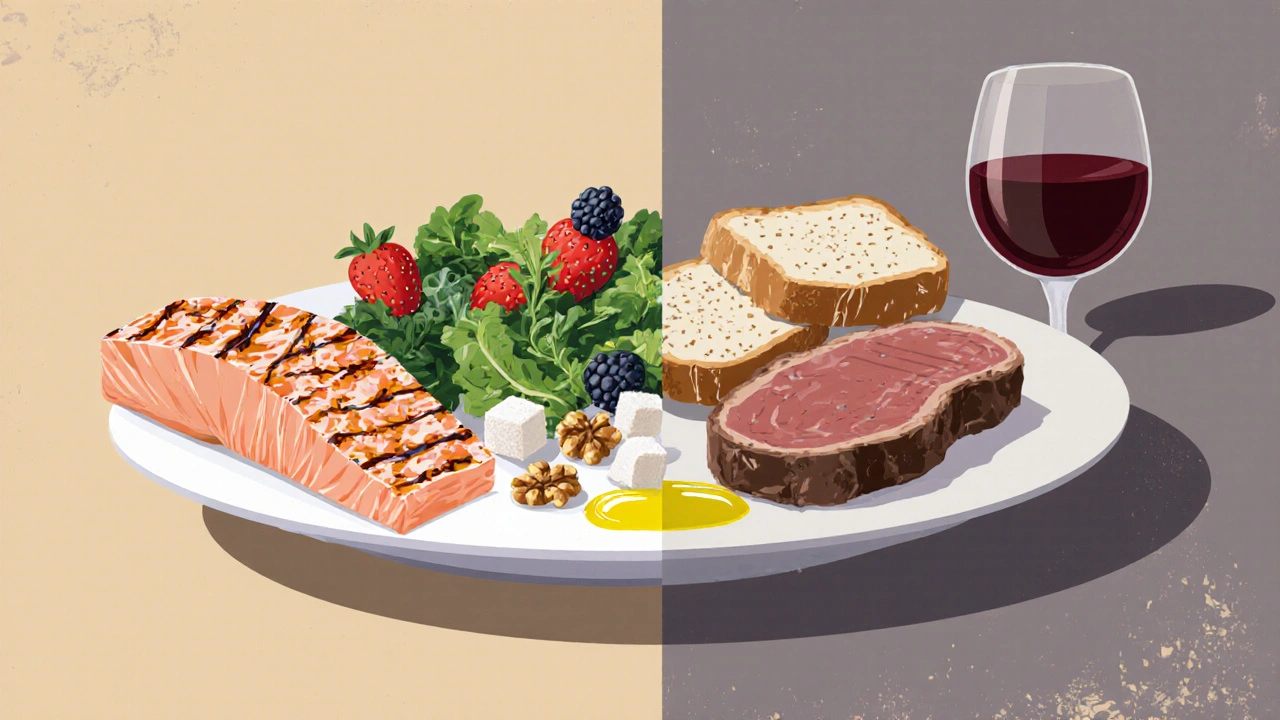
Key Foods to Embrace
Below is a quick‑reference list of nutrient powerhouses that consistently show benefits in clinical and observational studies.
- Fatty fish - salmon, mackerel, sardines (rich in EPA and DHA omega‑3s).
- Leafy greens - kale, spinach, Swiss chard (loaded with antioxidants like lutein).
- Seeds & nuts - chia, flaxseed, walnuts (extra plant‑based omega‑3s and fiber).
- Colorful berries - blueberries, strawberries, raspberries (vitaminC and polyphenols).
- Olive oil - extra‑virgin version supplies oleocanthal, an anti‑inflammatory compound.
- Probiotic foods - kefir, yoghurt, kimchi, sauerkraut (support gut‑skin axis).
- VitaminD‑rich foods - fortified dairy, eggs, mushrooms exposed to UV light.
These foods are not just "nice to have"; they actively shift your body’s inflammatory profile. Aim for at least two servings of fatty fish per week, a daily handful of berries, and a spoonful of flaxseed mixed into breakfast smoothies or oatmeal.
Common Triggers to Limit or Eliminate
Everyone’s body reacts a bit differently, but research pinpoints a handful of culprits that repeatedly show up in psoriasis flare‑up diaries.
| Eat More | Avoid |
|---|---|
| Fatty fish (salmon, mackerel) | Processed sugars (sodas, candy) |
| Leafy greens (kale, spinach) | Refined carbs (white bread, pastries) |
| Seeds & nuts (walnuts, chia) | Excess saturated fats (fry‑ups, fatty cuts of red meat) |
| Berries & citrus (vitaminC boost) | Gluten‑containing grains (wheat, barley) for sensitive individuals |
| Probiotic foods (kimchi, kefir) | Nightshade vegetables (tomatoes, peppers) if you notice worsening symptoms |
| VitaminD‑rich foods (fortified milk, UV‑treated mushrooms) | Alcohol in large quantities (can increase inflammation) |
Why these foods matter:
- Processed sugar spikes insulin, which in turn ramps up inflammatory cytokines.
- Saturated fats raise LDL cholesterol and can worsen skin scaling.
- Gluten may trigger an autoimmune response in a subset of psoriasis patients, especially those with celiac disease.
- Nightshades contain solanine, a compound that some people find irritates skin.
Putting It All Together: Sample 3‑Day Meal Plan
Planning ahead removes the guesswork and keeps you from reaching for fast‑food comfort during a flare‑up. Below is a realistic menu that balances nutrients, flavor, and convenience.
- Day1
- Breakfast: Greek yoghurt topped with blueberries, a drizzle of honey, and 1tbsp ground flaxseed.
- Lunch: Spinach salad with grilled salmon, avocado, walnuts, and olive‑oil‑lemon dressing.
- Dinner: Stir‑fried broccoli, carrots, and tofu in ginger‑garlic sauce, served over quinoa.
- Snack: A small apple and a handful of almonds.
- Day2
- Breakfast: Oatmeal cooked with fortified almond milk, mixed berries, and a pinch of cinnamon.
- Lunch: Turkey wrap using a gluten‑free tortilla, mixed greens, sliced cucumber, and hummus.
- Dinner: Baked mackerel with lemon‑dill, side of sautéed kale, and sweet‑potato mash.
- Snack: Carrot sticks with probiotic‑rich kefir dip.
- Day3
- Breakfast: Smoothie with spinach, frozen strawberries, banana, chia seeds, and oat milk.
- Lunch: Lentil soup (low‑sodium) paired with a side salad dressed in olive oil.
- Dinner: Grilled chicken breast, quinoa pilaf with pumpkin seeds, and roasted Brussels sprouts.
- Snack: A small piece of dark chocolate (70%cocoa) and a cup of green tea.
Notice the repetition of anti‑inflammatory staples (fatty fish, greens, seeds) and the absence of obvious triggers. Feel free to swap proteins or vegetables based on personal preferences, as long as the core nutrient balance stays intact.

Practical Tips for Sticking to the Psoriasis Diet
- Shop the perimeter - Fresh produce, seafood, and dairy are usually found along the grocery store’s outer aisles.
- Batch‑cook - Prepare a big pot of lentil soup or roasted veggies on Sunday; portion them for the week.
- Read labels - Watch out for hidden sugars in sauces, dressings, and “low‑fat” items that often add more sugar.
- Hydrate - Aim for 2‑3L of water daily; proper hydration supports skin barrier function.
- Track symptoms - Keep a simple journal noting meals and flare‑up severity; patterns emerge faster than you think.
When to Seek Professional Guidance
Diet alone isn’t a cure, but it can be a powerful adjunct to medical treatment. If you notice any of the following, talk to a dermatologist or a registered dietitian:
- Rapid worsening of plaques despite dietary changes.
- New joint pain that could signal psoriatic arthritis.
- Signs of nutrient deficiency (persistent fatigue, brittle nails).
Personalized nutrition plans consider your age, activity level, and any co‑existing conditions such as diabetes or heart disease.
Frequently Asked Questions
Can a gluten‑free diet improve psoriasis?
For some patients, especially those with celiac disease or non‑celiac gluten sensitivity, cutting gluten can reduce inflammation and clear skin. However, evidence is mixed, so try a short 4‑week trial and monitor symptoms before making it permanent.
Do omega‑3 supplements work if I can’t eat fish?
High‑quality fish oil capsules (containing EPA≥500mg per serving) have been shown to decrease plaque thickness in several trials. Plant‑based alternatives like algae oil provide DHA, though EPA levels may be lower.
Is dairy bad for psoriasis?
Full‑fat dairy can be inflammatory for some, but low‑fat, calcium‑rich options such as kefir and fortified plant milks often supply vitaminD and probiotics without the excess saturated fat.
How quickly can I see skin improvements after changing my diet?
Most people notice a reduction in itching and redness within 2‑4weeks, but visible plaque thinning may take 8‑12weeks. Consistency is key; occasional cheat meals won’t ruin progress.
Should I avoid nightshade vegetables completely?
Only if you’ve personally flagged them as triggers. Many patients tolerate tomatoes and peppers without issue, so test them one at a time and keep a symptom log.
Lindy Swanson
Look, I get the hype around “psoriasis diet” but I’ve seen dozens of fad plans that promise miracles and end up just being pricey kale smoothies. The science isn’t black‑and‑white, and throwing out entire food groups can backfire on your gut microbiome. If you’re still buying the hype, you might be missing the bigger picture of overall lifestyle.
Amit Kumar
Totally hear you, Lindy! 😊 It’s easy to get lost in the noise, but sticking to the core anti‑inflammatory foods like salmon, spinach, and berries really does help calm the flare‑ups. Even a tiny daily sprinkle of flaxseed can make a difference. Keep rocking that balanced approach!
Crystal Heim
Focus on omega‑3 rich fish and leafy greens they reduce cytokine storms the evidence is solid practical foods work better than gimmicks
Sruthi V Nair
When you examine the diet from a systems view the body is a network of signals each meal either amplifies or dampens the inflammatory cascade thus meals rich in antioxidants become a form of quiet meditation for cells
Mustapha Mustapha
Hey folks, just a quick note – if you’re trying this plan, aim for consistency. Prep your meals on Sunday, keep a water bottle handy, and don’t forget to listen to how your skin reacts after each week. Small tweaks add up.
Ben Muncie
Honestly, I think the moral of the story is that you don’t need to become a monk to eat better. A couple of fish servings a week and swapping soda for water is enough for most people.
kevin tarp
Just a heads‑up: the article’s list mixes processed and whole foods without clear distinction. When you write about nutrition, separate “raw” from “refined” to avoid confusion.
ravi kumar
In my country we have centuries‑old spices that naturally curb inflammation – turmeric, cumin, coriander – they’re not just flavor boosters but biochemical allies; ignoring indigenous wisdom in a “global” diet guide feels like a missed opportunity and a subtle erasure of cultural heritage.
SandraAnn Clark
Food is fuel but also a vibe, so if you’re feeling blah, try berries instead of chips – simple switch, simple win.
Rex Wang
Honestly, the tip about staying hydrated is spot‑on; water supports skin barrier function, and sipping regularly can reduce dryness – a small habit with big payoff!
mark Lapardin
From a mechanistic standpoint, the intersection of diet and psoriasis hinges on several immunometabolic pathways. First, omega‑3 polyunsaturated fatty acids, predominantly EPA and DHA sourced from fatty fish, act as substrates for resolvin and protectin synthesis, which in turn downregulate NF‑κB signaling and limit the release of pro‑inflammatory cytokines such as IL‑17 and IL‑23. Second, dietary antioxidants-including lutein, zeaxanthin, and various flavonoids found in leafy greens and berries-mitigate oxidative stress by scavenging reactive oxygen species, thereby preventing keratinocyte hyperproliferation. Third, the gut‑skin axis plays a pivotal role: probiotics and prebiotic fibers foster a diverse microbiota, leading to increased production of short‑chain fatty acids like butyrate, which strengthen intestinal barrier integrity and reduce systemic endotoxemia. Fourth, vitamin D, whether obtained from fortified dairy or UV‑treated mushrooms, modulates T‑cell differentiation, promoting regulatory T cells over Th17 cells, an effect directly relevant to the pathogenesis of psoriasis. Fifth, saturated fats and refined carbohydrates induce post‑prandial hyperglycemia, which spikes insulin and amplifies mTOR signaling, a pathway known to exacerbate skin plaque formation. Sixth, gluten may act as a molecular mimic for certain epidermal antigens in genetically susceptible individuals, triggering cross‑reactive immune responses; however, this effect appears to be limited to a subset of patients with concurrent celiac disease or non‑celiac gluten sensitivity. Finally, alcohol consumption elevates circulating acetaldehyde and disrupts hepatic metabolism of retinoids, further compromising skin barrier repair. In practice, a layered dietary approach-prioritizing omega‑3 rich seafood, antioxidant‑dense produce, fermented probiotic foods, and adequate vitamin D while limiting processed sugars, saturated fats, and alcohol-creates a synergistic anti‑inflammatory milieu. Clinical trials have demonstrated modest reductions in PASI scores (Psoriasis Area and Severity Index) after 12 weeks of such an intervention, reinforcing the translational relevance of these nutritional strategies. Nonetheless, individual variability necessitates personalized monitoring; patients should maintain a symptom‑food journal to identify idiosyncratic triggers and adjust macronutrient ratios accordingly. In summary, while diet alone is not a cure, its integration with pharmacologic therapy can enhance therapeutic outcomes, improve quality of life, and potentially reduce reliance on systemic immunosuppressants.
Barry Singleton
The data suggest that omega‑3 supplementation yields a statistically significant, albeit modest, reduction in PASI scores, but one must consider confounding variables such as adherence, baseline diet quality, and polypharmacy. Moreover, the gut‑skin axis hypothesis remains under‑explored in large‑scale cohorts.
Javier Garcia
Curious whether a low‑FODMAP twist would help anyone with gut‑related flare‑ups.
christian quituisaca
Great question, Javier! A low‑FODMAP approach can ease bloating and gut irritation, which might indirectly calm skin inflammation for some folks. It’s worth experimenting with a short trial while tracking your skin’s response.
Donnella Creppel
Okay, listen up-if you think you can just eat kale and call it a day, you’re missing the nuance. The diet world isn’t a monolith; it’s a mosaic of personal biochemistry, cultural heritage, and yes, even a dash of luck. So, stop pretending there’s a one‑size‑fits‑all solution and start tailoring your plate to YOUR body.
Jarod Wooden
While the kale‑only paradigm is reductionist, the epistemic framework for integrative nutrition demands a dialectic synthesis of macro‑ and micronutrients, lest we succumb to reductionist fallacies.
lee charlie
I hear you both. Finding what works can feel like trial and error, but logging meals and symptoms can reveal patterns that guide smarter choices.
Greg DiMedio
Sure, logging is fun…
Badal Patel
My dear compatriots, permit me to elucidate the gravitas of this discourse; indeed, the very fabric of culinary tradition intertwines with dermatological destiny-one must, with due reverence, adopt a regimen that honors both heritage and science.
KIRAN nadarla
While the prose is ornate, the practical takeaway remains: balance omega‑3 intake, limit refined sugars, and monitor individual responses-standard recommendation.





Write a comment