QT Prolongation Risk Calculator
Your Risk Assessment
Risk Assessment Results
Key Risk Factors
Every year, hundreds of people die suddenly from a heart rhythm problem they never knew they were at risk for - and in many cases, it wasn’t their heart that failed. It was a medication they took for something else. QT prolongation isn’t a disease you feel. It doesn’t show up on a routine checkup. But when it goes wrong, it can trigger a deadly arrhythmia called Torsades de Pointes, which can lead to sudden cardiac death in minutes. The good news? We know which drugs cause it. We know who’s most at risk. And we know how to prevent it - if we’re looking.
What QT Prolongation Really Means
The QT interval on an ECG measures how long it takes your heart’s lower chambers to recharge after each beat. When that interval stretches too long - longer than 450 milliseconds in men, or 470 in women - your heart becomes electrically unstable. That’s QT prolongation. It doesn’t always cause symptoms. Many people have no idea their QT is prolonged until something triggers a dangerous rhythm. The problem isn’t the length alone. It’s how fast it changes. A rise of more than 60 milliseconds from your baseline is a red flag. And when the T-wave gets tall and broad, or splits into two peaks, that’s when the risk of Torsades de Pointes spikes. This isn’t theoretical. In the ARIC study of over 10,000 adults, every one standard deviation increase in T-wave duration raised the risk of sudden death by 21%.Medications That Can Trigger This
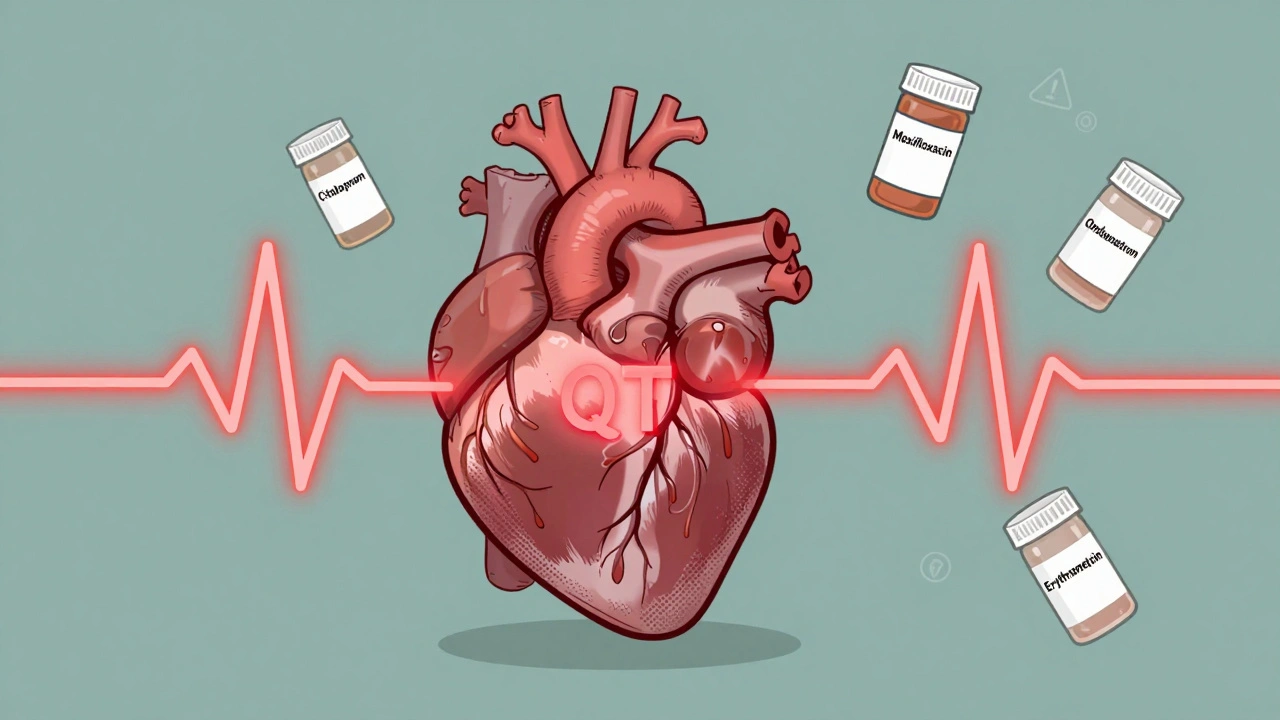
Over 100 common prescription drugs can prolong the QT interval. Some are obvious - antiarrhythmics like sotalol and dofetilide. But many others are everyday meds people take without thinking. Antibiotics like moxifloxacin can add 6-15 milliseconds to the QT interval. Erythromycin? It doubles the risk of sudden cardiac death, especially if you’re also taking a drug that blocks the CYP3A4 enzyme - like grapefruit juice, some antifungals, or even certain antidepressants. That combo can push the risk up fivefold. Antidepressants vary wildly. Citalopram at 40 mg daily adds about 8.5 milliseconds. Escitalopram at the same dose? Just 4.2. That’s not a small difference - it’s the difference between a warning and a red alert. Antipsychotics like haloperidol and ziprasidone are also high-risk. Even the anti-nausea drug ondansetron, often given in ERs, can prolong QT in vulnerable people. The FDA has flagged 142 medications with QT-related warnings. That’s nearly 9% of all prescription drugs. And it’s not just the drug itself. It’s what else you’re taking.Who’s Most at Risk?
It’s not just about the medication. It’s about you. Women are more susceptible than men - partly because their baseline QT is naturally longer. Older adults are at higher risk too. People over 65 take an average of 7.8 medications. Nearly one in three of them is on at least one QT-prolonging drug. Combine that with age-related kidney or liver changes, and the body can’t clear the drug properly. Toxicity builds up quietly. Low potassium or magnesium? That’s a major amplifier. Correcting potassium to above 4.0 mEq/L cuts QT-related risk by 62%. Low magnesium? That’s another trigger. Even mild dehydration can make things worse. Heart disease changes everything. If you’ve had a heart attack, have heart failure, or have thickened heart muscle, your risk of drug-induced arrhythmia jumps 10 to 100 times. The American Heart Association says structural heart disease is the biggest amplifier of risk - bigger than the drug itself. Genetics matter too. Some people carry silent mutations in genes like KCNQ1 or HERG that make them extra sensitive. The NIH’s All of Us program is now collecting genetic data from a million people to find these hidden risks. But right now, we can’t test for them routinely.
The Hidden Danger: Drug Interactions
One drug might be safe alone. Two together? Deadly. CYP3A4 inhibitors - drugs that slow down how your liver breaks down other meds - are the silent killers here. Common ones include clarithromycin, ketoconazole, fluconazole, and even some HIV meds. Take erythromycin with one of these? Risk skyrockets. Antidepressants and antifungals? Dangerous mix. Antipsychotics with anti-nausea meds? High risk. Even over-the-counter antacids like cimetidine can interfere. Most doctors don’t check for these combinations unless they’re specialists. And most patients don’t know to mention every pill they take - including supplements. A 2022 study at a major U.S. hospital found that 78% of automated QTc alerts were false positives. That’s alarm fatigue. Clinicians start ignoring them. But the real danger is when the one true alarm slips through.What Doctors Should Do - And What They Often Don’t
The MHRA and other health agencies recommend a simple three-step check before prescribing:- Check the patient’s baseline QTc. If it’s already over 450 (men) or 470 (women), think twice.
- Look for electrolyte imbalances. Check potassium, magnesium, and calcium levels.
- Review every other medication. Use a tool like AZCERT.org - updated weekly - to see which drugs interact.
What You Can Do
If you’re on any of these meds - antidepressants, antibiotics, antipsychotics, anti-nausea drugs - ask your doctor:- Is my QT interval checked? When was the last ECG?
- Am I on any other drugs that could interact?
- Have my potassium and magnesium levels been checked recently?
- Is there a safer alternative?
The Future: Better Tools, Smarter Care
New tech is helping. In 2023, the FDA approved QTguard by Verily - an AI system that analyzes ECGs and cuts false alarms by 53%. It doesn’t just measure the QT interval. It looks at the shape of the T-wave, the timing, even the noise in the signal. That’s a game-changer. The International Council for Harmonisation now requires new drugs to be tested for T-wave changes - not just QTc. That’s more accurate. It means fewer drugs will be pulled off the market after people die. But the biggest advance is personalization. The NIH’s All of Us project is building a database of genetic and health data from a million people. Someday, your DNA might tell your doctor: “This drug is safe for you. That one isn’t.” Until then, we rely on the basics: check the ECG, check the labs, check the list of meds.Bottom Line
QT prolongation isn’t a mystery. It’s a measurable, preventable risk. Most cases of sudden cardiac death linked to drugs happen because no one looked. No one asked. No one checked. You don’t need to be a cardiologist to save a life. You just need to know: QT prolongation is real. It’s silent. And it’s preventable.Can a normal ECG rule out risk for QT prolongation?
No. A single ECG only shows your heart’s state at that moment. QT intervals can change with electrolyte levels, heart rate, or drug accumulation. Someone with a normal QT today could develop prolongation days later if they start a new medication or become dehydrated. Regular monitoring is key for high-risk patients.
Are over-the-counter drugs or supplements risky for QT prolongation?
Yes. Some OTC antihistamines like diphenhydramine (Benadryl) and herbal supplements like St. John’s Wort can prolong QT. Even high doses of zinc or licorice root can lower potassium, indirectly increasing risk. Always tell your doctor about everything you take - including vitamins and teas.
If I have a family history of sudden death, should I get genetic testing?
If you have a close relative who died suddenly before age 50 without clear cause - especially during exercise or sleep - genetic testing for inherited long QT syndrome may be warranted. But for most people, the risk comes from medications, not genes. Talk to a cardiologist if you’re unsure.
Can QT prolongation be reversed?
Yes, often. Stopping the offending drug, correcting low potassium or magnesium, and treating underlying conditions like heart failure can normalize the QT interval within days. In severe cases, doctors may give magnesium sulfate IV or use a pacemaker to speed up the heart rate and shorten the QT.
Why do some people have no symptoms even with severe QT prolongation?
Because Torsades de Pointes doesn’t always happen. The heart can stay in a prolonged state for weeks without triggering a deadly rhythm. Risk depends on multiple factors: how long the QT is, how fast the heart beats, whether there’s heart damage, and even stress or sleep patterns. That’s why it’s so hard to predict - and why prevention is everything.
For those on long-term medications, the safest approach isn’t fear - it’s awareness. Know your meds. Know your numbers. Ask the questions. One conversation could be the difference between a routine follow-up and a life saved.
Saket Modi
Bro, I took azithromycin last year and felt like my heart was gonna explode. Didn't think twice. Now I just avoid all antibiotics like they're cursed. 🤡
Chris Wallace
I've been a nurse for 18 years and I still see this happen. Someone gets prescribed an antibiotic for a sinus infection, takes it with their antidepressant, and then ends up in the ER with a weird flutter. It's not dramatic. It's quiet. And that's why it's so dangerous. Nobody's screaming. Nobody's panicking. Just a slow, silent electrical glitch in a body that's been overmedicated for years. And then-poof. Gone. We need better systems, not just alerts that everyone ignores.
william tao
The clinical data presented here is both compelling and, frankly, alarming. One must acknowledge the profound epidemiological implications of polypharmacy-induced QT prolongation, particularly in the context of CYP3A4-mediated pharmacokinetic interactions. The absence of standardized genomic screening protocols represents a critical lacuna in contemporary preventive cardiology.
John Webber
i had no idea so many pills could do this. i take citalopram and sometimes benadryl when i got a cold. now im scared to even take tylenol. maybe i should just stop all meds and live in the woods?
Shubham Pandey
Stop taking random meds. Check your K and Mg. Done.
Elizabeth Farrell
I want to say thank you for writing this with such care. I’ve watched my mom go through three different antidepressants because her doctor never checked her QT or her electrolytes. She ended up in the hospital after a simple UTI treatment with a drug she’d been on for years. It wasn’t the infection-it was the combo. Since then, we keep a little card in her wallet: "QT caution: citalopram, azithromycin, omeprazole." Simple. Clear. Life-saving. If you’re on more than three meds, please, please ask your pharmacist to run a drug interaction check. It takes two minutes. And it might save your life.
Sheryl Lynn
Ah, yes-the modern pharmacopeia: a symphony of unintended consequences, orchestrated by pharmaceutical titans who’ve turned the human body into a Rube Goldberg machine of metabolic cross-talk. One mustn't forget that the QT interval is not merely a number-it's a poetic sigh of the myocardium, a whispered elegy for the over-medicated soul. And yet, we still reach for the pill as if it were a sacrament.
Paul Santos
Fascinating stuff. The QT interval as a biomarker of pharmacological entropy-truly a meta-physiological phenomenon. I mean, think about it: we’re measuring the *recovery phase* of cardiac repolarization, which is essentially the heart’s way of saying, "I’m tired, bro." And then we throw in fluconazole and grapefruit juice like it’s a cocktail. 🍊⚡️
Eddy Kimani
I work in a rural clinic and we don’t have automated QT alerts. We just eyeball ECGs and hope for the best. But I started asking every patient over 50: "What else are you taking? Even the stuff you think doesn’t matter?" I found three people on QT-prolonging combos they didn’t even know about. One guy was taking St. John’s Wort with sertraline and didn’t think it counted as a "drug." We changed his meds. He’s fine now. Small changes. Big impact.
Chelsea Moore
I CAN’T BELIEVE THIS ISN’T A TV SPECIAL!! THIS IS THE MOST IMPORTANT THING NO ONE IS TALKING ABOUT!! MY COUSIN DIED AT 32 FROM A "HEART ATTACK" AND SHE WAS ON ZOLOFT AND ANTIBIOTICS!! WHY ISN’T THE GOVERNMENT FORCING PHARMACIES TO PRINT WARNING STICKERS ON EVERY QT-PROLONGING MED?? I’M STARTING A PETITION!!
John Biesecker
you ever think about how weird it is that we trust pills more than our own bodies? we swallow chemicals like they’re magic beans, then panic when something goes wrong. maybe the real problem isn’t the drugs-it’s that we’ve forgotten how to listen. the heart doesn’t lie. if you feel off, stop. breathe. check your potassium. talk to someone. it’s not about fear. it’s about paying attention. 🌱❤️
Genesis Rubi
USA has the best healthcare in the world. If you die from a drug interaction, you probably just didn’t take enough responsibility. We don’t need more warnings-we need more discipline. And maybe stop taking so many foreign meds. Seriously, who lets a doctor prescribe something from a country that doesn’t even have FDA? 🇺🇸





Write a comment