Choosing Between Warfarin and DOACs Isn’t Just About Effectiveness - It’s About Your Life
If you’re on a blood thinner, you’re not just taking a pill. You’re managing a daily balancing act between preventing a stroke or clot and avoiding a dangerous bleed. For decades, warfarin was the only game in town. Today, direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran have taken over as the go-to choice for most people. But that doesn’t mean warfarin is obsolete. In fact, for some, it’s still the safest option. Understanding the real differences - not just the marketing - can make all the difference in your health.
Why DOACs Took Over: Simplicity Wins
Warfarin requires constant monitoring. You need regular blood tests - INR checks - to make sure your dose is just right. Too low, and you’re at risk for clots. Too high, and you could bleed internally without warning. Many people get tested 6 to 12 times in the first month, then every few weeks after that. That’s a lot of doctor visits, needle sticks, and stress.
DOACs changed all that. They work reliably without routine blood tests. You take a fixed dose - once or twice a day - and that’s it. No need to track vitamin K intake from leafy greens. No need to worry about interactions with antibiotics or painkillers. In 2023, DOACs made up nearly 78% of all anticoagulant prescriptions in the U.S. Apixaban alone (sold as Eliquis) was prescribed over 25 million times globally that year.
The reason? Convenience. A 2023 study in the American Journal of Managed Care found that DOAC users had 32% higher adherence rates than warfarin users. For people under 45, that gap jumped to 41%. When you don’t have to think about your medication every week, you’re more likely to take it - and that’s the biggest safety factor of all.
Real Safety Differences: Bleeding Risk Is the Deciding Factor
Both types of drugs prevent clots. But which one causes fewer serious bleeds? The data is clear: DOACs win.
A 2024 study in the American Heart Association Journal showed that DOACs reduced the risk of major bleeding by 28% compared to warfarin. The biggest difference? Intracranial hemorrhage - bleeding in the brain. DOACs cut that risk by about 50%. That’s huge. A brain bleed is often deadly or permanently disabling. Warfarin’s unpredictable nature makes it far more likely to cause this kind of disaster.
Among DOACs themselves, safety varies. Apixaban consistently shows the lowest bleeding rates. In a 2022 Blood Advances study, apixaban had a 42% lower risk of severe bleeding than rivaroxaban. Dabigatran was better at preventing recurrent clots, while edoxaban offered a middle ground. So even within DOACs, not all are equal.
When Warfarin Is Still the Best Choice
DOACs aren’t perfect. They fail in three key situations where warfarin remains the only proven option.
- Mechanical heart valves: DOACs are strictly contraindicated here. Studies show they increase the risk of valve clots and death. Warfarin is the gold standard - and has been for 70 years.
- Severe kidney failure (eGFR below 15): Most DOACs are cleared through the kidneys. When kidney function is this low, the drugs can build up dangerously. Warfarin, processed by the liver, doesn’t have this issue.
- Severe mitral stenosis: This rare heart valve condition requires precise anticoagulation. Only warfarin has been tested and proven safe here.
For these patients, warfarin isn’t outdated - it’s essential. The American College of Chest Physicians and the European Society of Cardiology both still recommend it as first-line therapy in these cases.
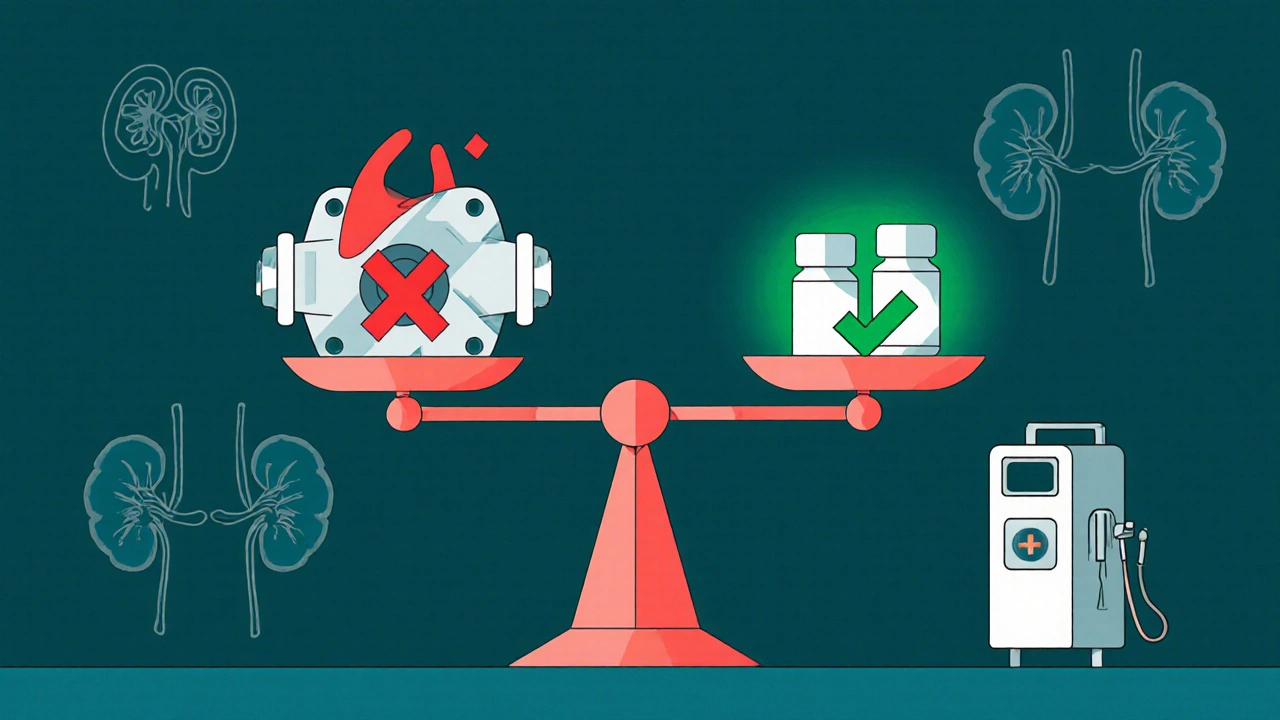
What About Kidney Problems? It’s More Complex Than You Think
Many assume DOACs are unsafe if you have kidney disease. That’s not true - but it’s not simple either.
DOACs work fine down to a creatinine clearance (CrCl) of 25 mL/min. Below that, safety drops. Dabigatran is the most affected - 80% of it leaves the body through the kidneys. Apixaban? Only 27%. That’s why apixaban is often the preferred DOAC for people with moderate kidney impairment.
Here’s the twist: A 2023 study in JAMA Network Open found that for patients with eGFR below 60, extended DOAC use actually carried a higher bleeding risk than warfarin. That’s why doctors often lower the DOAC dose in these patients - but not always. Standard doses are still recommended for most, unless kidney function is very poor.
For dialysis patients, the data is still emerging. The 2023 KDIGO guidelines say warfarin may be safer here, but newer studies show DOACs can reduce bleeding by 29% in advanced kidney disease. This is a gray area - and your nephrologist should be part of the decision.
Cost Is a Real Barrier - But Not Always What You Think
Warfarin costs about $4.27 for a 30-day supply. Apixaban? Around $587. Rivaroxaban? $523. That’s a huge difference. Many patients assume DOACs are too expensive to be worth it.
But here’s what the data doesn’t show: the hidden costs of warfarin. Those INR tests? Each one can cost $50-$100. Add in doctor visits, time off work, and emergency trips for bleeding episodes, and the total cost over a year can easily exceed $2,000 - even with insurance.
Plus, Medicare claims data shows that 35% of warfarin users miss at least one INR test per month. That’s not just inconvenient - it’s dangerous. When patients fall out of the therapeutic range, their risk of stroke or bleed spikes. DOACs eliminate this risk entirely. A 2023 Circulation study found that DOACs became cost-effective when warfarin adherence dropped below 65%. That’s the reality for many.
Reversing Bleeds: What Happens If You Start Bleeding?
This is a common fear. What if you fall and start bleeding internally? Can the drug be reversed?
Warfarin can be reversed with vitamin K and fresh frozen plasma, but it takes hours to work. DOACs have specific antidotes now. Idarucizumab (Praxbind) reverses dabigatran in minutes. Andexanet alfa (Andexxa) reverses apixaban and rivaroxaban. These are not magic bullets - they’re expensive and used only in emergencies - but they exist. Warfarin doesn’t have a fast-acting, targeted antidote.
For most people, this won’t matter. But if you’re at high risk for falls, or live alone, knowing reversal options exist can be a relief.
What About Diet and Other Medications?
Warfarin is famously sensitive to diet. Vitamin K - found in kale, spinach, broccoli - directly opposes warfarin’s effect. One week of eating a lot of greens, then switching to salads every day, can throw your INR off. That’s why people on warfarin are told to eat the same amount of vitamin K every day. It’s exhausting.
DOACs? No dietary restrictions. You can eat whatever you want. Same with most medications. Warfarin interacts with over 300 drugs - from antibiotics to herbal supplements like St. John’s wort. DOACs have fewer interactions, but they’re not zero. NSAIDs like ibuprofen can still increase bleeding risk with any anticoagulant. Always check with your doctor before starting a new pill.
Who Should Switch? Who Should Stay?
Here’s a simple guide based on current guidelines and real-world outcomes:
- Switch to a DOAC if: You have atrial fibrillation (not caused by a mechanical valve), normal or mild kidney function, and struggle with frequent blood tests or dietary restrictions.
- Stay on warfarin if: You have a mechanical heart valve, severe kidney failure (eGFR <15), severe mitral stenosis, or have been stable on warfarin for years with excellent INR control.
- Consider apixaban first: Among DOACs, it has the lowest bleeding risk and works well even with moderate kidney issues.
- Avoid standard-dose DOACs if: Your weight is under 60 kg and your kidney function is borderline. Your doctor may need to reduce the dose - but never reduce it without testing.
What’s Next? The Future of Blood Thinners
Research is moving fast. A new drug called Librexia™ - a combination of warfarin and vitamin K - is in phase 3 trials. It’s designed to stabilize INR levels and eliminate the need for frequent testing. If it works, it could bring back warfarin for a new generation.
Meanwhile, the AUGUSTUS-CKD trial is tracking over 2,000 patients with advanced kidney disease and atrial fibrillation. Results are expected by late 2024. That could finally settle the debate about DOACs in dialysis patients.
One thing’s certain: The era of warfarin as the default is over. But it’s not gone. It’s just become more specialized. The best anticoagulant isn’t the newest one - it’s the one that fits your body, your lifestyle, and your risks.
Are DOACs safer than warfarin for most people?
Yes, for most people with atrial fibrillation or deep vein thrombosis, DOACs are safer. They reduce the risk of major bleeding - especially brain bleeds - by nearly 30% compared to warfarin. They also don’t require frequent blood tests or dietary restrictions, which improves adherence and overall safety.
Can I switch from warfarin to a DOAC on my own?
No. Switching requires careful planning. Your doctor must check your kidney function, review your medications, and time the transition to avoid gaps in protection or dangerous overlap. Never stop or switch anticoagulants without medical supervision.
Why is apixaban often recommended over other DOACs?
Apixaban has the lowest rate of major bleeding among DOACs, especially in older adults and people with moderate kidney impairment. It’s also less affected by body weight and drug interactions. In clinical trials, it consistently outperformed rivaroxaban and dabigatran in safety without sacrificing effectiveness.
What if I can’t afford a DOAC?
Warfarin is still a valid option if you can manage the monitoring. Many clinics offer free or low-cost INR testing. Some pharmacies have patient assistance programs for DOACs. Talk to your doctor - there are options. But don’t skip doses or stop taking your medication just because of cost. That’s far riskier.
Do DOACs work the same for everyone?
No. DOACs vary by kidney function, weight, age, and other medications. Dabigatran is cleared mostly by the kidneys, so it’s riskier if your kidneys are weak. Apixaban is safer in older adults and those with lower body weight. Your doctor picks the right DOAC and dose based on your individual profile - not a one-size-fits-all approach.
Final Thought: Your Safety Depends on the Right Fit
There’s no single best anticoagulant. The right one is the one that matches your health, your body, and your life. For most, DOACs are simpler, safer, and more effective. But for those with mechanical valves or failing kidneys, warfarin still saves lives. Don’t let cost or convenience override medical need. Talk to your doctor. Ask about your kidney numbers. Ask about bleeding risks. Ask what happens if you miss a dose. The answers will guide you to the safest choice - not the trendiest one.
Shawn Daughhetee
I switched from warfarin to apixaban last year and honestly my life changed
I used to dread my monthly blood tests and always worried about eating spinach
Now I just take my pill and forget about it
Best decision I ever made
Miruna Alexandru
The data is compelling but the framing is misleading. DOACs aren't inherently safer-they're statistically safer in controlled populations with ideal adherence. Real-world outcomes are messier. Many patients on DOACs have undiagnosed renal decline, leading to accumulation and unanticipated bleeding. The 'convenience' narrative ignores the silent erosion of clinical vigilance. We're trading monitoring for molecular opacity.
Justin Daniel
Man I used to be on warfarin and it was a nightmare
Every time I ate a salad I’d panic
Then I switched to Eliquis and it was like getting my life back
Don’t get me wrong-warfarin’s still vital for some folks
But if you’re not on a mechanical valve? DOACs are a gift
Melvina Zelee
i just wanna say that i love how this post breaks it down like this
so many people think its just 'newer = better' but no
its about your body your lifestyle your kidneys your wallet
i had a cousin on warfarin who missed her tests and ended up in the er with a bleed
she switched to apixaban and now she hikes every weekend
its not magic its just better fit
steve o'connor
I'm Irish and we're big on warfarin here still. Lots of older folks. But I've seen the shift. My uncle with AFib went from monthly blood draws to a once-daily pill. He said it felt like being trusted again. No more 'did you eat kale?' lectures. The reversal drugs? Still pricey, but knowing they exist? That's peace of mind.
ann smith
This is such an important topic 💙
So many people feel overwhelmed by anticoagulants
But understanding the real differences? It empowers you
And if you're struggling with warfarin? Please talk to your doctor about DOACs
You deserve to live without constant fear
And yes-your kidney function matters, but so does your peace of mind 😊
Julie Pulvino
I'm on rivaroxaban and I didn't even know there were different types of DOACs until I read this
Turns out apixaban is better for bleeding risk
My doc just gave me the first one that came up
Guess I'm gonna ask for a switch
Also-why is warfarin still $4? That feels like a typo
Daniel Jean-Baptiste
i read this and thought about my dad who has a mechanical valve
he's been on warfarin for 15 years
he says the INR tests are annoying but he'd never switch
he says he knows his body now
and if something goes wrong he knows what to do
thats worth something
Jessica Correa
The cost thing hit me hard
My insurance covers DOACs but my copay is $75
Warfarin is $5
But then I did the math on all the tests and missed work
Turns out I'm spending more on warfarin
So I switched
Best $75 I ever spent
Nikhil Chaurasia
In India, warfarin is still king because DOACs are too expensive
But I've seen people die because they couldn't afford INR tests
Or they skipped them because they couldn't take time off work
It's not about which drug is better
It's about which system supports you
And ours doesn't
Holly Schumacher
I'm a nurse. I've seen 3 patients die from DOAC-related bleeds because their doctors didn't adjust for renal decline. The marketing says 'no monitoring needed'-but that's a trap. You're just moving the risk from the lab to the ER. This post is dangerously oversimplified. DOACs are not safer. They're just less visible until they're catastrophic.
Michael Fitzpatrick
I’ve been on warfarin for over a decade because I have mitral stenosis and my cardiologist says DOACs are a no-go, but I’ve watched my friends switch and it’s been life-changing for them. The freedom from dietary tracking, the lack of constant needle pokes, the confidence that they’re not flying blind-it’s not just convenience, it’s dignity. I’m happy for them, even if I can’t join them. And yes, I still get my INR every 3 weeks, but I’ve learned to love the routine. It’s my rhythm now. I don’t resent it. I just wish the system made it easier for people who can’t afford the luxury of a DOAC.
james lucas
i just wanna say i got on apixaban after a stroke scare and honestly
the biggest thing was not having to think about it
no more counting spinach
no more wondering if my antibiotic messed with my dose
and i know people say oh but what if you bleed
but i also know i can go to the er and they have a pill to undo it
in minutes
warfarin wouldve taken hours
and if you're alone like me
that matters
manish chaturvedi
In India, we don't have access to DOACs for most people. Warfarin is the only option. But the real issue isn't the drug-it's the lack of infrastructure. INR machines are scarce. Labs are hours away. People skip tests because they can't afford the bus fare. This isn't a debate about pharmacology-it's about equity. Until we fix that, 'safety' is a luxury word.






Write a comment