
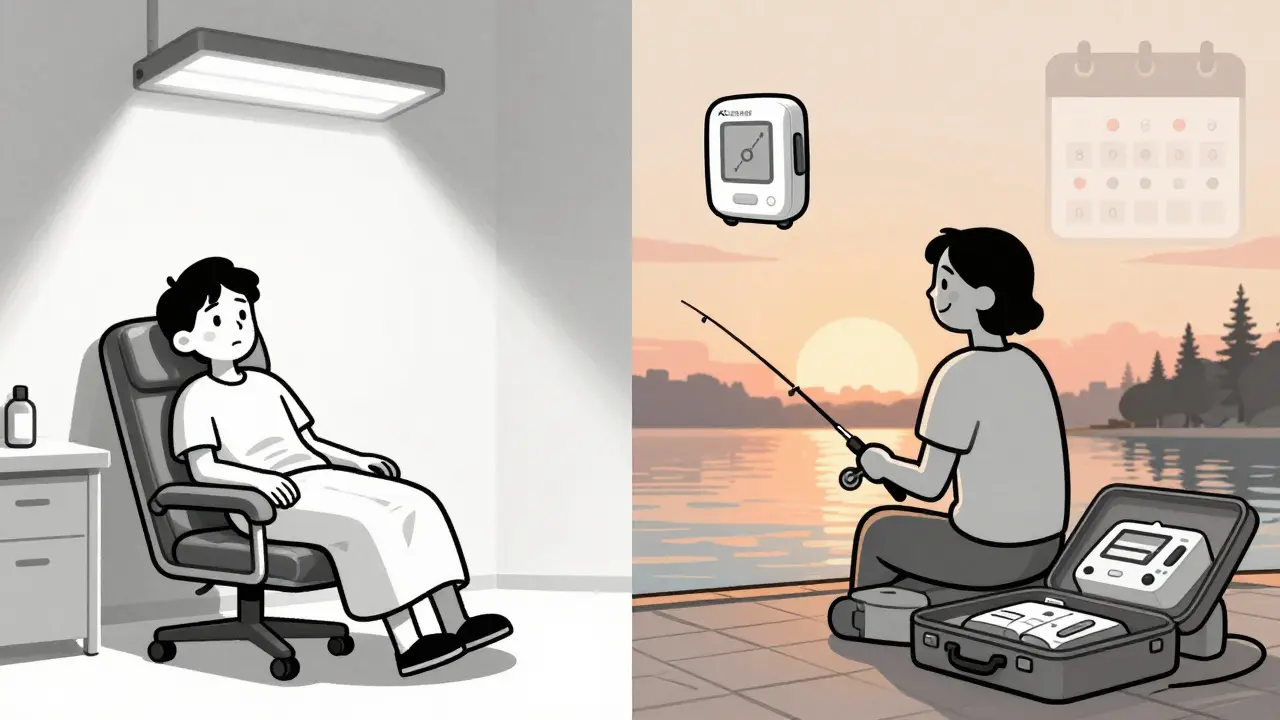
For someone living with end-stage renal disease, the idea of dialysis doesn’t just mean medical treatment-it means hours spent in a clinic, rigid schedules, and a life shaped around machines and appointments. But there’s another path: home hemodialysis. It’s not for everyone, but for those who qualify, it changes everything. No more commuting three times a week. No more waiting for a machine. No more feeling like a patient in a system instead of a person in control of their own care.
What Home Hemodialysis Actually Looks Like
Home hemodialysis means doing your dialysis treatment in your own space-on your couch, in your bedroom, even while you sleep. The machines are smaller than they used to be, and modern systems like the NxStage System One or Fresenius 5008 are designed for home use. But it’s not just about moving the machine. It’s about learning how to handle every step yourself-or with help from someone you trust.You’ll need a dedicated space, roughly 6 feet by 6 feet, to store supplies, set up the machine, and have room for your care partner. Plumbing matters too. You need a dedicated drain line and a water line that delivers 40-80 psi pressure. Most homes can handle this with minor upgrades. Electricity? A dedicated 120-volt, 20-amp circuit is required. No sharing outlets with the fridge or microwave.
Water quality is non-negotiable. Your machine uses purified water, and that means your home system must meet AAMI standards. Monthly water and dialysate cultures, annual chemical testing, and daily logs of chlorine levels aren’t optional. They’re part of the safety checklist every home dialysis patient follows.
Training Isn’t a One-Week Course-It’s a Commitment
Most people assume training for home hemodialysis takes a few days. It doesn’t. It takes weeks. On average, it’s 4 to 6 weeks, but some programs stretch to 12 weeks. The U.S. Medicare system covers up to 25 training sessions, which gives you room to learn at your own pace.Training isn’t just watching a nurse. You’ll practice setting up the machine, priming tubing, connecting your vascular access, and inserting needles-your own. Self-needling is the biggest hurdle for nearly half of trainees. Many programs now use virtual reality simulators to build confidence before touching skin. At the University of Washington, this approach raised competency rates from 78% to 92%.
Your care partner goes through the same training. No exceptions. They learn how to handle alarms, check blood pressure, respond to low blood pressure or air in the line, and when to call for help. In most cases, you cannot dialyze alone. The Maryland Department of Health and other major programs require a trained partner to be present during every session. That’s a hard reality for about 30% of potential candidates who don’t have someone reliable to help.
Training ends with written and practical exams. You must show you can troubleshoot a leak, recognize signs of infection at your access site, and log every treatment accurately. If you miss a step, you go back. No shortcuts.
Three Ways to Schedule Your Treatments
Home hemodialysis isn’t one-size-fits-all. You get to choose your schedule-and that choice affects your health more than you might think.- Conventional home hemodialysis: Three times a week, 3-4 hours per session. This looks like in-center dialysis, but you do it on your own time-early morning, late night, or even on weekends. It’s the easiest transition for beginners.
- Short daily home hemodialysis: Five to seven times a week, 2-3 hours each. This is where real benefits kick in. Studies show a 28% lower risk of death compared to in-center dialysis. Blood pressure improves. Fluid overload drops. Left ventricular mass shrinks. You feel less tired. One patient in Sydney told me, “I used to nap after dialysis. Now I play with my grandkids.”
- Nocturnal home hemodialysis: While you sleep. Three to seven nights a week, 6-10 hours per session. This gentle, slow removal of waste and fluid is the gold standard for phosphate control. Patients on nocturnal dialysis reduce their phosphate binder pills by an average of 3.2 per day. That’s a lot of pills gone. And because it’s slow, you rarely get cramps or low blood pressure.
The longer and more frequent the sessions, the better the outcomes. But they also demand more time, more energy, and more commitment. Not everyone can do six nights a week. But even doing four short sessions a week can make a measurable difference.

Outcomes: Why This Isn’t Just About Convenience
People think home dialysis is about comfort. It’s more than that. It’s about survival.According to the U.S. Renal Data System, home hemodialysis patients have a 15-20% lower mortality rate than those on in-center dialysis-even after adjusting for age, diabetes, and other health issues. The advantage is strongest with frequent or nocturnal schedules. A 2018 study in Nephrology Dialysis Transplantation found nocturnal patients had 42% lower phosphate levels. That means less bone disease, fewer heart problems, and less need for medications.
Quality of life jumps, too. A 2019 review in the American Journal of Kidney Diseases showed home patients scored 37% higher on quality-of-life surveys. Why? More energy. Fewer dietary restrictions. Less time stuck in a chair. One man in Ohio said, “I started fishing again. I didn’t realize how much I missed it.”
But it’s not all smooth sailing. On forums like Reddit and the American Association of Kidney Patients, common complaints include machine alarms (67% of users), managing supplies (58%), and the emotional toll of relying on a care partner (52%). Some relationships strain under the pressure. Others grow stronger. It depends on communication, patience, and support.
Barriers Still Stand in the Way
Despite the benefits, home hemodialysis remains rare. Only 12% of U.S. dialysis patients use it. Why? Because most clinics don’t offer it. The National Institute of Diabetes and Digestive and Kidney Diseases found only 12% of dialysis centers have home training programs. That’s a geographic barrier for many.Even when programs exist, staffing is an issue. Nephrologists say 71% of centers lack enough trained nurses to run home programs. Medicare pays for training, but not enough to cover the staff time needed. That’s why some centers limit spots or require patients to pay for extra sessions.
Then there’s the fear. Most people are scared of needles, machines, and emergencies. That’s normal. But training isn’t about being fearless. It’s about being prepared. Programs that focus on competency-proving you can handle a problem-rather than just ticking off days, see far fewer complications in the first year.
What’s Changing Now
The tide is turning. In 2021, the Advancing American Kidney Health initiative set a goal: 80% of new ESRD patients should start dialysis at home or with a transplant by 2025. We’re nowhere near that. But progress is happening.New machines are smaller, smarter, and easier to use. The WavelinQ endoAVF system, approved in 2022, creates a more reliable access point with less risk of infection. The NxStage System One is now approved for more types of patients, including those with heart conditions.
And in 2025, Medicare is changing how it pays. Instead of paying the same amount whether you dialyze at home or in a center, payments will tie to outcomes-like blood pressure control, hospitalizations, and survival. That shift will make home dialysis more financially attractive for clinics and more accessible for patients.
Is It Right for You?
Home hemodialysis isn’t a downgrade from in-center care. It’s an upgrade-if you’re ready for it. You need:- A reliable care partner (or a plan for solo treatment, which is rare and requires extra approval)
- Space in your home for equipment and supplies
- Good mental and physical health to manage the routine
- Willingness to learn, practice, and ask for help
If you’re considering it, talk to your nephrologist. Ask if your clinic offers home training. Ask about their success rates. Ask how many patients complete training and stay on home dialysis after a year. Don’t settle for a quick answer. This isn’t a decision you make in five minutes.
For many, home hemodialysis means regaining control. It means sleeping through the night without alarms. It means having dinner with family without rushing to a clinic. It means living-not just surviving.
Can you do home hemodialysis alone?
In most cases, no. Safety guidelines require a trained care partner to be present during every treatment. Solo home hemodialysis is possible with special equipment and approval, but it’s rare and only offered to a small group of highly trained patients with no history of dizziness, seizures, or cognitive issues. Most programs won’t approve it unless you’ve been on home dialysis successfully for over a year with a partner first.
How long does home hemodialysis training take?
Training typically lasts 4 to 6 weeks, but it can range from 3 to 12 weeks depending on your learning pace, the type of machine, and whether you’re learning self-needling. Medicare covers up to 25 training sessions, so you have time to practice. Some centers use virtual reality simulators to speed up the process, especially for needle insertion.
What’s the difference between short daily and nocturnal home hemodialysis?
Short daily hemodialysis means 5-7 sessions per week, each lasting 2-3 hours, done during the day. Nocturnal means 3-7 sessions per week, each lasting 6-10 hours, done while you sleep. Nocturnal is gentler and more thorough-it clears toxins and fluid slowly, which reduces cramps and improves phosphate control. Short daily is easier to fit into a daytime schedule and still offers major health benefits.
Does home hemodialysis cost more than in-center?
No. Medicare and most private insurers cover home hemodialysis at the same rate as in-center dialysis. In fact, because you avoid travel and hospitalizations, your overall healthcare costs may be lower. The machine and supplies are provided by the dialysis company, and you don’t pay for clinic fees. The only extra cost might be water or electricity, which is minimal.
Can you travel with a home hemodialysis machine?
It depends on the machine. Standard home hemodialysis machines are not portable. If you travel, you’ll need to arrange treatments at a clinic near your destination. But the NxStage System One is portable-you can take it in a suitcase. You’ll still need to plan ahead: bring supplies, check water quality at your destination, and arrange for power. Many patients do this successfully with careful preparation.
What if my care partner gets sick or can’t be there?
You need a backup plan. That means identifying a second trained person-a friend, relative, or even a home health aide-who can step in. Some patients train two partners. If no one is available, you may need to temporarily switch back to in-center dialysis until your partner returns. Never skip a session without consulting your care team.
How do I know if I’m a good candidate for home hemodialysis?
You’re a good candidate if you’re motivated, have a reliable care partner, can follow complex routines, and are willing to learn. Your doctor will check your physical health, mental readiness, home setup, and social support. The most important factor isn’t your kidney function-it’s your ability to handle stress and stay consistent. Many people who are physically strong fail because they underestimate the emotional load.
If you’re considering home hemodialysis, start by asking your nephrologist for a referral to a home dialysis program. Don’t wait for them to bring it up. Be the one to say, “I want to explore this option.” The system isn’t perfect, but for many, home dialysis isn’t just a treatment-it’s a return to life.
Linda Caldwell
Just did my 4th nocturnal session and I slept through the whole thing-no cramps, no nausea, woke up ready to make pancakes for my grandkids. This isn’t treatment, it’s life back.
Radhika M
In India, home dialysis is rare because of cost and water quality. But if you have clean water and a helper, it’s possible. Start small-learn one step at a time.
Naomi Lopez
The notion that home hemodialysis is merely a ‘convenience’ is a gross oversimplification. It’s a radical reclamation of bodily autonomy in a system designed to depersonalize chronic illness. The clinical data is robust, yet the infrastructure remains pathetically underfunded. This isn’t healthcare innovation-it’s healthcare resistance.
CAROL MUTISO
Oh wow, so we’re supposed to be impressed that people are now doing the bare minimum of staying alive in their own homes? How noble. Meanwhile, the system still makes you train for six weeks just to not die in your living room. Bravo, capitalism.
Jessica Salgado
I trained for 11 weeks. Learned to self-need. My partner cried the first time I stuck myself. We both did. But now? I changed my own tubing at 2 a.m. while watching The Crown. That’s power. That’s dignity. That’s not just surviving-it’s living on my terms.
Erik J
Does the NxStage System One require a specific type of water filter? I’ve read conflicting info about reverse osmosis vs. deionization in home setups.
Salome Perez
As someone who’s walked alongside three loved ones through this journey, I’ve seen the quiet heroism of home dialysis. It’s not glamorous. It’s not loud. But it’s the gentlest form of rebellion against a system that treats kidneys like disposable parts. You don’t just learn to operate a machine-you learn to hold space for your own humanity.
Raven C
...And yet, despite all the data, the emotional labor, the logistical nightmares, the *sacrifice*-the system still treats this as a ‘niche option.’ How quaint. How tragically, bureaucratically, *unimaginative*.
Evelyn Vélez Mejía
There is a philosophical truth here: medicine has long treated the body as a machine to be fixed, not a life to be lived. Home hemodialysis, in its quiet, meticulous, demanding form, forces a reckoning. It asks: Who gets to define ‘normal’? Who gets to decide when treatment becomes living? The answer, increasingly, is the patient-and that, above all, is the revolution.




Write a comment