Getting the right dose of medication isn’t just about following the label. For many people, the standard dose on the bottle could be too much-or too little-depending on their age, weight, and how well their kidneys are working. Too high a dose can lead to dangerous side effects. Too low, and the drug won’t work. This isn’t guesswork. It’s science. And it’s happening every day in hospitals, clinics, and pharmacies around the world.
Why One Size Doesn’t Fit All
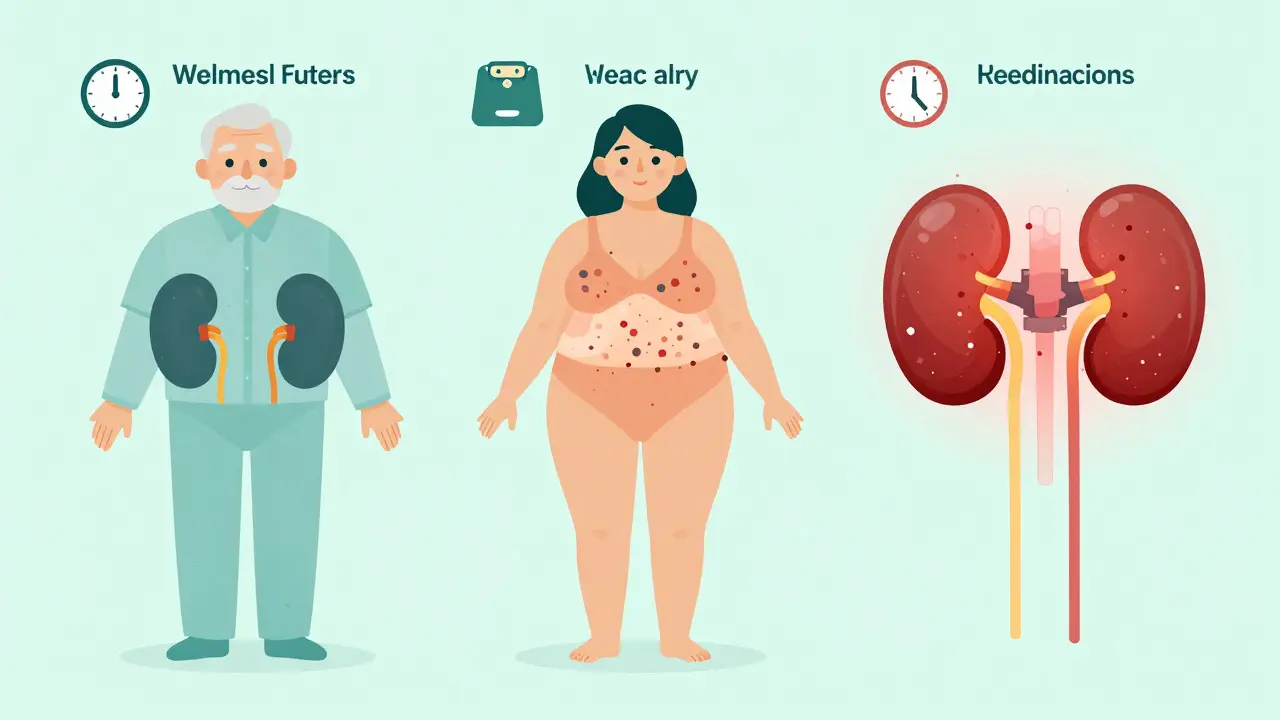
Think of your body like a car. The same gas pedal setting might get you to 60 mph on a flat road, but uphill, you need more power. Your kidneys act like the engine’s exhaust system-they filter out drugs so they don’t build up. But if that system is slow, clogged, or worn out, the same dose can turn toxic.That’s why doctors and pharmacists look at three key things: how old you are, how much you weigh, and how well your kidneys are filtering waste. These aren’t just numbers. They’re signals that tell the body how to handle medicine.
Age Changes How Your Body Handles Drugs
As you get older, your body changes. Muscle mass drops. Fat increases. Your liver and kidneys don’t work as fast. Even if your blood tests look normal, your body might clear drugs more slowly.Take a common painkiller like acetaminophen. In a healthy 30-year-old, it’s gone from the body in about 4 hours. In someone over 70, that time can stretch to 8 hours or more. That means if you keep taking the same dose, you’re slowly building up a dangerous amount.
Same goes for antibiotics, blood pressure pills, and diabetes meds. A 2020 study in the American Journal of Kidney Diseases found that nearly 30% of serious drug reactions in older adults happened because their kidneys couldn’t clear the medicine fast enough. The problem? Many prescriptions aren’t adjusted for age.
That’s why guidelines now say: if you’re over 65, assume your kidney function is reduced-even if your creatinine levels look fine. Doctors should check your estimated glomerular filtration rate (eGFR) before prescribing anything that’s cleared by the kidneys.
Weight Matters-More Than You Think
If you’re underweight, your body has less space to spread out the drug. That means even a normal dose can hit you harder. If you’re overweight, the drug might get trapped in fat tissue and never reach the target area.For example, vancomycin, a powerful antibiotic used for serious infections, needs careful dosing. In a person with a BMI over 30, using their actual weight can lead to under-dosing. The drug gets diluted in extra fat and muscle, so the bloodstream doesn’t get enough. That’s why doctors use something called adjusted ideal body weight.
Here’s how it works: First, calculate your ideal body weight. For men, it’s 50 kg + 2.3 kg for every inch over 5 feet. For women, it’s 45.5 kg + 2.3 kg per inch over 5 feet. Then, if you’re obese, you don’t use your full weight. You use: ideal weight + 0.4 × (actual weight - ideal weight).
That small tweak can mean the difference between a cure and a relapse. A 2019 study showed that using actual weight in obese patients led to 15-20% overestimation of kidney function, which meant doses were too low. Patients stayed sick longer. Some even developed resistant infections.

Kidney Function: The Hidden Factor
Your kidneys filter about 120-150 quarts of blood each day. When they slow down, drugs stick around. That’s why kidney function is the most critical factor in dosing.Most doctors use a number called eGFR-estimated glomerular filtration rate. It’s calculated from your age, sex, race, and blood creatinine level. The standard formula today is the CKD-EPI equation, adopted by the National Kidney Foundation in 2009 and updated in 2012.
Here’s what the numbers mean:
- eGFR ≥90: Normal kidney function
- eGFR 60-89: Mild reduction
- eGFR 45-59: Mild to moderate reduction
- eGFR 30-44: Moderate to severe reduction
- eGFR 15-29: Severe reduction
- eGFR <15: Kidney failure
For most drugs, no adjustment is needed if your eGFR is above 60. Between 30 and 59, many medications need lower doses or longer gaps between doses. Below 30, almost all kidney-cleared drugs require major changes.
But here’s the catch: eGFR is great for diagnosing kidney disease. But for dosing, many drug labels still use an older formula called the Cockcroft-Gault equation, which estimates creatinine clearance (CrCl) in mL/min. Why? Because most drug studies from the 1980s and 90s used CrCl. So even though eGFR is more accurate for staging kidney disease, doctors still need CrCl for dosing.
This creates confusion. One lab gives you eGFR. The drug guide says CrCl. You have to convert. And if you get it wrong? You risk harm.
What Drugs Need the Most Attention?
Not all drugs are affected the same way. Some are mostly cleared by the kidneys. Others are broken down by the liver. The ones that are risky? They’re often the ones you take every day.Antibiotics: Vancomycin, cefazolin, ciprofloxacin. Too low? Infection doesn’t clear. Too high? Kidney damage or hearing loss.
Diabetes meds: Metformin. If your eGFR drops below 30, it’s contraindicated. Even at eGFR 30-45, many doctors cut the dose in half. A Reddit user shared a near-miss: someone was taking 1000 mg twice daily with an eGFR of 28. The max safe dose? 500 mg once a day.
Heart meds: Digoxin, lisinopril, furosemide. All cleared by kidneys. Overdose can cause irregular heartbeat, low blood pressure, or severe dehydration.
Pain meds: Gabapentin, pregabalin. These don’t cause liver damage, but they build up in the blood if kidneys slow down. Result? Dizziness, confusion, falls.
A 2022 survey of pharmacists found that 68% saw incorrect kidney dosing at least once a week. Antibiotics were the top offender-followed by heart and diabetes drugs.
How Do You Know What to Do?
It’s not up to you to calculate this. But you can ask the right questions.- “Is this dose based on my kidney function?”
- “Do you know my eGFR or creatinine clearance?”
- “Is this dose adjusted for my weight?”
- “Can you check if this drug needs a change because I’m over 65?”
Ask for a copy of your latest kidney function test. If you don’t have one, ask for one. Many people don’t realize their creatinine level was checked during a routine blood test.
Pharmacists are your best ally. They have access to databases like Lexicomp and Micromedex that list exact dosing adjustments for hundreds of drugs based on eGFR and weight. If your doctor prescribes something new, ask your pharmacist to review it.
And if you’re on multiple meds? Ask for a medication review. Many clinics offer free reviews for seniors or people with chronic conditions.
Technology Is Helping-But It’s Not Perfect
Hospitals are starting to use electronic alerts. When a doctor orders a drug, the system checks your eGFR and weight, then flags if the dose is wrong. A 2019 study showed this cut serious errors by 47%.But automated systems aren’t flawless. One doctor in Boston told a Medscape interview that his system once recommended cutting an antibiotic dose so much that it failed to treat a life-threatening infection. The algorithm didn’t know the patient had sepsis-the body needed a full dose to survive.
That’s why human judgment still matters. Algorithms give you a starting point. Your doctor or pharmacist has to decide if it’s right for your situation.
Soon, things will get even smarter. The NIH is funding AI tools that will combine kidney function with genetics, age, weight, and even gut health to predict the perfect dose. Pilot programs start in late 2024. But for now, the best tool is still a well-informed patient and a careful provider.
What You Can Do Today
You don’t need to be a doctor to protect yourself. Here’s what works:- Know your eGFR. Ask for it at your next checkup.
- Keep a list of all your meds-prescription, over-the-counter, and supplements.
- Ask your pharmacist: “Does this need a kidney or weight adjustment?”
- If you’re over 65 or have diabetes or high blood pressure, assume your kidneys aren’t working at 100%-and ask if your doses need changing.
- Report side effects: dizziness, confusion, nausea, swelling, or unusual fatigue. These could be signs of drug buildup.
Medication safety isn’t about following instructions blindly. It’s about understanding how your body works-and making sure your pills match it.
How do I know if my medication dose needs to be adjusted for my kidneys?
Your doctor or pharmacist should check your estimated glomerular filtration rate (eGFR), which comes from a simple blood test measuring creatinine. If your eGFR is below 60 mL/min/1.73m², many drugs need lower doses or longer dosing intervals. Always ask: “Is this dose safe for my kidney function?” and request a copy of your latest eGFR result.
Does being overweight mean I need a higher dose of medication?
Not always. For some drugs like antibiotics (vancomycin) or antifungals, using your actual weight can lead to under-dosing because the drug gets diluted in fat tissue. In these cases, doctors use adjusted ideal body weight: ideal weight + 0.4 × (actual weight − ideal weight). But for other drugs, like statins or blood pressure pills, weight doesn’t change the dose. It depends on how the drug moves through your body.
Why do some drug labels use Cockcroft-Gault and others use eGFR?
The Cockcroft-Gault equation estimates creatinine clearance (CrCl) and was used in most drug trials from the 1970s to 2000s. So drug labels still reference it. The eGFR equation (CKD-EPI) is more accurate for diagnosing kidney disease, but it’s not directly used for dosing. Many hospitals now calculate both and convert eGFR to CrCl for dosing purposes to avoid confusion.
Can I just take the same dose if I feel fine?
No. Feeling fine doesn’t mean your body is handling the drug correctly. Many drugs that build up slowly-like gabapentin or metformin-don’t cause symptoms until damage is done. A person with low kidney function might feel normal while their blood levels of the drug are dangerously high. Regular kidney checks and dose reviews are essential, even if you feel okay.
What should I do if my doctor won’t adjust my dose?
Ask for a referral to a clinical pharmacist or nephrologist. Many hospitals have medication therapy management programs that specialize in complex dosing. Bring your lab results and a list of all your medications. If your doctor dismisses your concerns, get a second opinion. Medication safety is your right-not a suggestion.
Medication dosing isn’t magic. It’s math, biology, and careful attention. When age, weight, and kidney function are ignored, people get hurt. When they’re respected, treatments work better and side effects drop. You don’t need to be an expert-but you do need to ask the questions. Your life could depend on it.
Anjula Jyala
Standard dosing protocols are a joke in clinical practice. eGFR is a flawed metric-race correction is pseudoscience and still embedded in most algorithms. Creatinine is useless in sarcopenic elderly. You need cystatin C. If your hospital doesn’t use it, you’re practicing 1990s medicine. No one adjusts for muscle mass. No one. Just slap on a number and hope.
Pharmacists are the only ones who read the guidelines. Doctors? They click ‘default dose’ and move on.
Kirstin Santiago
This is such an important topic. So many people don’t realize that meds aren’t one-size-fits-all, especially as we age or if we’re managing chronic conditions. I’ve seen friends on the same meds as their siblings but have completely different reactions. It’s not about being weak or strong-it’s biology. And honestly, the fact that we still rely so much on weight and creatinine alone is kind of scary. We need better tools.
Thank you for breaking this down clearly.
Kathy McDaniel
omg i just realized my grandpa’s blood pressure med was probably too strong for him 😅 he’s 82 and always says he feels ‘zombie-like’ after taking it. maybe his kidneys are slow? i’m gonna ask his dr about eGFR next visit. thanks for the nudge!!
Patrick Merrell
People think medicine is exact science. It’s not. It’s a gamble with side effects. You take a pill, hope it works, and pray your kidneys aren’t failing. The system is broken. Doctors are overworked. Pharmacies are profit-driven. And patients? They’re just numbers on a screen. No wonder so many end up in the ER from ‘correctly prescribed’ meds.
Stop pretending this is safe. It’s not.
Conor Flannelly
There’s a philosophical layer here that rarely gets discussed. If we accept that biology is unique to each individual, then why do we still design drugs and dosing protocols as if we’re all the same? It’s a relic of industrial medicine-batch production applied to human physiology.
Our bodies aren’t widgets. We’re complex, dynamic systems shaped by genetics, environment, lifestyle, even stress. The fact that we reduce all this to age, weight, and creatinine feels almost arrogant. We need personalized medicine, not just personalized dosing.
It’s not just science. It’s humility.
Conor Murphy
I’ve been on anticoagulants for years and my dose has changed 3 times just because my weight shifted 10 lbs. It’s wild how sensitive these things are. One day you’re fine, next day you’re dizzy or bruising like crazy. It’s not ‘just a pill.’ It’s a delicate dance with your body.
Also-yes, kidney function matters more than people think. I had a routine blood test that looked ‘normal’ but my eGFR was 52. My dr didn’t even mention it until I asked. That’s the problem.
Desaundrea Morton-Pusey
Why are we even talking about this? In America we have the best doctors, the best labs, the best tech. If your meds aren’t working, you’re probably not following instructions. Or worse-you’re one of those people who thinks ‘natural remedies’ are better than science.
Stop making excuses. Take your pill. Stop blaming your kidneys.
Kegan Powell
Love this breakdown. Seriously. The weight thing blew my mind. I’m 6’1” and 240 lbs and I always thought ‘normal dose’ meant normal for me. Turns out my fat tissue was hiding the drug like a secret stash.
Adjusted ideal body weight? That’s genius. Why isn’t this taught in med school? Why isn’t it automatic in e-prescribing systems?
We need better software. Not just better doctors.
April Williams
Of course your kidneys matter. But what about the fact that 70% of elderly patients are on 5+ medications? Polypharmacy is a silent killer. No one looks at drug interactions. No one checks if the blood pressure med makes the diabetes med less effective. It’s a disaster waiting to happen.
And don’t even get me started on how pharmacies just refill everything automatically. No one’s paying attention. You’re lucky if you live past 70.
Harry Henderson
THIS IS WHY WE NEED MEDICAL REVOLUTION. Not tweaks. Not ‘guidelines.’ We need AI-driven dosing algorithms that pull from real-time biometrics. Wearables. Continuous kidney monitoring. Genetic profiles. We’re in 2025 and we’re still guessing based on a blood test from last year?
It’s criminal. Wake up, healthcare.
suhail ahmed
Man, this hits different coming from India. We’ve got patients on full adult doses at 45kg because the doctor says ‘it’s the same pill.’ No adjustments. No labs. No eGFR. Just ‘take one.’ I’ve seen people collapse from tylenol overdose because they were told ‘it’s safe.’
We need to stop treating poor countries like they’re just ‘lower-resource’ versions of the West. They’re different. Their bodies are different. Their access is different.
This isn’t just science-it’s justice.
Candice Hartley
My mom’s creatinine was normal but her eGFR was 48. Dr didn’t adjust her statin. She got rhabdo. Took 3 months to recover.
Always ask for eGFR. Always.
astrid cook
Oh great. Another ‘science’ post that makes people feel guilty for being old or fat. Like we’re somehow failing our bodies. Newsflash: aging isn’t a choice. Obesity isn’t always about laziness. And not everyone can afford fancy labs.
Stop virtue signaling with eGFR. Fix the system.
Andrew Clausen
Correction: the CKD-EPI equation was updated in 2021, not 2012. The 2009 version included race coefficients. The 2021 update removed them. Your post is outdated. And you didn’t mention the new 2021 serum creatinine-based equation without race. That’s critical.
Accuracy matters. This isn’t opinion. It’s data.






Write a comment