When your hip starts hurting, it’s easy to blame a bad workout or sleeping funny. But if the pain sticks around - especially when you sit, squat, or twist - it might be more than just soreness. Two common but very different conditions, labral tears and hip arthritis, often show up together and can make everyday movement feel like a chore. The good news? You don’t always need surgery. For many people, the most powerful tool is something you can start today: activity modification.
What’s Really Going On in Your Hip?
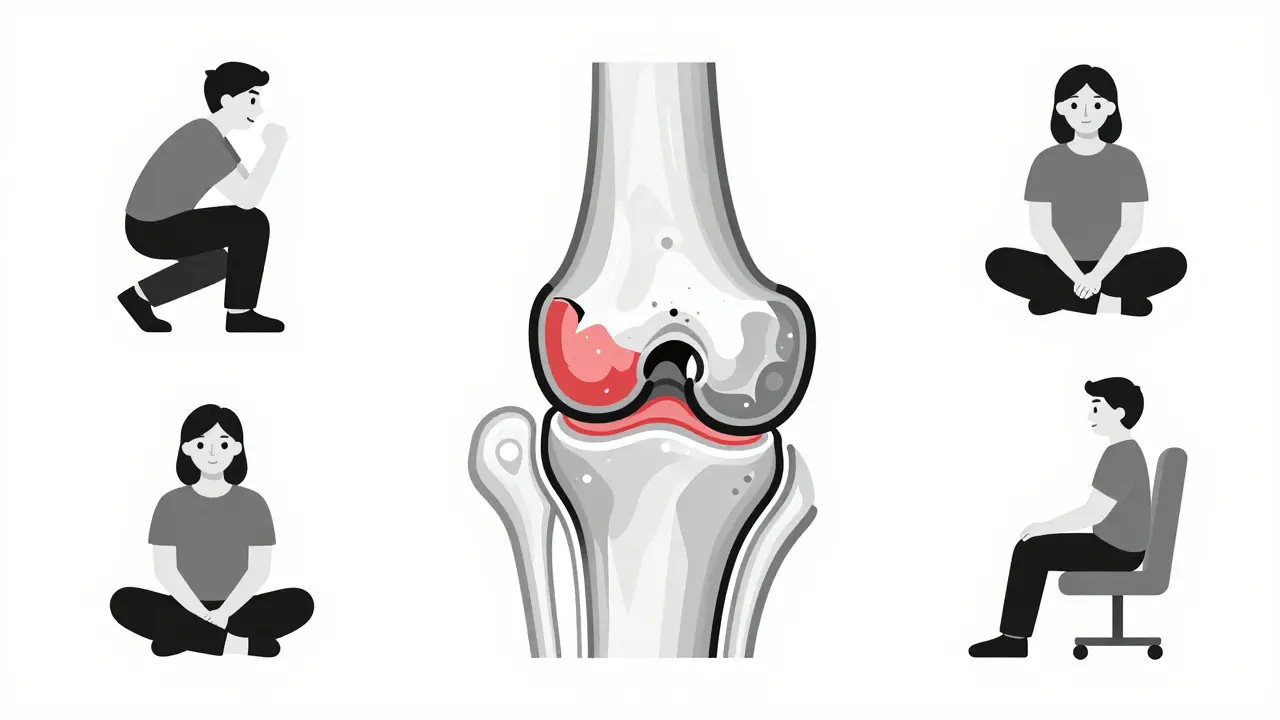
Your hip joint is a ball-and-socket, but it’s not as simple as it looks. Around the socket (acetabulum) is a ring of tough cartilage called the labrum. It’s about 3 to 5 millimeters thick, acts like a rubber seal, and helps keep your hip stable. When this labrum tears - often from repetitive twisting, deep squatting, or structural issues like cam impingement - it doesn’t just hurt. It lets joint fluid leak out, increasing pressure on the cartilage that covers the bones. That’s when arthritis can start to creep in. Hip osteoarthritis, on the other hand, is the slow breakdown of that smooth cartilage surface. It’s not just wear and tear - it’s inflammation, bone spurs, and joint space narrowing. Research shows that 70 to 90% of people with a labral tear also have signs of early arthritis. And 54% of those with hip arthritis have a torn labrum, even if they never had a specific injury. These aren’t separate problems. They feed each other.Labral Tears: More Than Just a “Pain Generator”
For years, doctors thought a torn labrum was just a source of pain. Now we know it’s a joint protector. Studies using cadavers show that when the labrum is damaged, contact pressure on the articular cartilage increases by 92%. That’s huge. A tear isn’t just a symptom - it’s a warning sign that your hip’s natural shock absorber is failing. Most labral tears happen in the front (anterior) of the hip - about 78% of cases. They’re often tied to femoroacetabular impingement (FAI), where bone grows abnormally on the ball or socket, causing them to bump into each other during movement. Cam-type FAI (excess bone on the ball) makes up 64% of cases. If you’re under 50 and have a labral tear, FAI is likely the root cause. But here’s the catch: 38% of people over 50 have labral tears on MRI - and feel zero pain. That means an image alone doesn’t tell the story. Pain matters more than pictures. If you’re not hurting, you don’t need surgery just because an MRI shows a tear.Arthritis: When the Joint Starts to Break Down
Hip arthritis progresses through four stages, measured by the Kellgren-Lawrence scale. Grade 0? No signs. Grade 4? Severe joint space narrowing (less than 2mm), bone-on-bone contact, and large bone spurs. Once you hit Grade 3 or 4, the cartilage is mostly gone. At that point, repairing the labrum won’t fix the deeper problem. That’s why treatment changes with age. If you’re 35 with a labral tear and early arthritis, repairing the labrum and fixing the impingement can delay surgery by years. But if you’re 65 with Grade 4 arthritis, the labrum isn’t the main issue - the cartilage is. Surgery on the labrum won’t stop the joint from wearing out. In fact, 45% of older patients with advanced arthritis end up needing a total hip replacement within five years, no matter what they try.Activity Modification: The Non-Surgical Game Changer
This is where most people get stuck. They think they have to choose between “do nothing” and “get surgery.” But there’s a third path: smart movement. Activity modification doesn’t mean quitting everything. It means changing how you move so your hip isn’t constantly stressed. The goal is to reduce pressure on the labrum and cartilage while keeping your muscles strong and your body moving. Here’s what works, based on real patient outcomes and clinical guidelines:- Avoid hip flexion beyond 90 degrees. That means no deep squats, no sitting in low chairs, no bending over to tie your shoes without bending your knees first.
- Limit internal rotation past 30 degrees. Cross-legged sitting? Gone. Pigeon pose in yoga? Modified or skipped.
- Don’t sit for more than 30-45 minutes at a time. Stand up, stretch, walk for a minute. Even a 5-minute walk every hour helps.
- Use a pillow between your knees when sleeping on your side. It keeps your hips aligned and reduces pressure on the joint.
- Switch from running to swimming or using an elliptical. These give you cardio without the pounding. One study found 71% of hip pain patients could stay active with swimming - only 29% could keep running.

What to Avoid - And What to Replace
Some activities are landmines for a bad hip:- Deep squats and lunges
- Running on hard surfaces
- Sitting cross-legged or in lotus position
- Stair climbing (especially going down)
- High-impact sports like basketball or tennis
- Swimming (freestyle and backstroke)
- Stationary cycling with high seat
- Elliptical trainer (low resistance)
- Water aerobics
- Walking on flat ground
Physical Therapy: The Missing Link
Activity modification alone isn’t enough. You need to rebuild strength where it matters most: your hip abductors (gluteus medius). Weak glutes force your hip to compensate, increasing stress on the labrum and cartilage. Physical therapy for hip pain focuses on:- Clamshells and side-lying leg lifts (80-100 degrees of hip flexion)
- Glute bridges with slow, controlled movement
- Core stability work to reduce pelvic tilt
- Teaching you to identify your personal “pain provocation positions”
When Other Treatments Help - And When They Don’t
NSAIDs like ibuprofen (400-800mg three times a day) can reduce inflammation and pain, but they don’t fix the root problem. Corticosteroid injections give temporary relief - about 3.2 months on average - but repeated use (more than three a year) carries a 12% risk of damaging cartilage further. Viscosupplementation (hyaluronic acid shots) helps some people with arthritis, but the benefit is modest: only 15-20% pain reduction in 55% of patients, and it fades after six months. The new FDA-approved Durolane lasts longer (up to six months), but it’s still not a cure. Surgery? Hip arthroscopy to repair a labral tear has a 85-92% satisfaction rate at five years - if you’re young, active, and have early arthritis. But if you’re over 60 with advanced joint damage, surgery doesn’t change the outcome much. The labrum might be fixed, but the cartilage is still gone.
The Invisible Disability
One of the hardest parts of hip pain isn’t the pain itself - it’s the misunderstanding. People don’t see it. You look fine. You’re not in a wheelchair. So they say, “Just move more!” or “You’re too young for that.” A survey from the Hospital for Special Surgery found that 68% of patients feel dismissed because their pain is invisible. That’s why education matters - for you, your family, your coworkers. This isn’t “just a bad hip.” It’s a biomechanical issue with real, measurable consequences.What’s Next? The Future of Hip Care
New tools are emerging. Wearable sensors that give real-time feedback on hip position during daily activities reduced pain episodes by 52% in a 2023 Stanford pilot study. Quantitative MRI can now spot cartilage damage before it shows up on regular X-rays. And the American Academy of Physical Medicine and Rehabilitation’s 2024 guidelines now stress “movement quality over quantity” - meaning how you move matters more than how much you move. The goal isn’t to stop living. It’s to keep moving - smarter. Early intervention with activity modification and targeted physical therapy can delay surgery by 3.5 to 5 years in 65% of patients with mild to moderate damage. But if you wait until the cartilage is gone, that window closes fast.Final Takeaway
Hip pain from labral tears and arthritis doesn’t have to mean surgery. It doesn’t mean giving up. It means learning how to move differently. You don’t need to be perfect. You just need to be consistent. Start today: sit higher, move slower, avoid deep bends, strengthen your glutes, and swap high-impact for low-impact. Track what hurts. Avoid it. Replace it. In three months, you might not be pain-free - but you’ll be in control.Can a labral tear heal on its own without surgery?
No, the labrum doesn’t heal on its own because it has poor blood supply. But that doesn’t mean you need surgery. Many people manage symptoms successfully with activity modification and physical therapy. The goal isn’t to repair the tear - it’s to stop it from causing more damage. If your pain improves with conservative care, surgery isn’t necessary.
Is walking good for hip arthritis?
Yes, walking is one of the best activities for hip arthritis - if done correctly. Walk on flat, even surfaces, wear supportive shoes, and keep your pace moderate. Avoid hills, uneven ground, or long distances if your pain flares. Walking helps maintain joint mobility, strengthens muscles, and reduces stiffness without putting excessive pressure on the joint.
Why does my hip hurt when I sit for too long?
Prolonged sitting increases pressure on the front of the hip joint, especially if your hips are flexed beyond 90 degrees. This compresses the labrum and irritates inflamed tissue. It also reduces circulation in the joint, leading to stiffness. Standing up every 30-45 minutes, even for a minute, helps reset the joint and relieve pressure.
Can I still exercise with a labral tear?
Absolutely - but you need to choose wisely. Avoid deep squats, lunges, and twisting motions. Focus on low-impact activities like swimming, cycling, elliptical training, and water aerobics. Strength training for your glutes and core is critical. Work with a physical therapist to design a safe routine. Movement keeps the joint nourished - inactivity makes things worse.
How do I know if I have a labral tear or just arthritis?
Pain location and triggers help. Labral tears often cause sharp, catching, or clicking pain in the front of the hip or groin, especially during twisting or deep flexion. Arthritis pain is usually deeper, more constant, and worse with weight-bearing. Imaging helps, but symptoms matter more. If you’re under 50 with activity-related pain, a labral tear is likely. If you’re over 60 with stiffness and pain at rest, arthritis is the bigger issue.
Will losing weight help my hip pain?
Yes - every pound lost reduces pressure on your hip joint by 3 to 4 pounds during walking. For someone with hip arthritis or a labral tear, even a 10-pound weight loss can significantly reduce pain and slow progression. Combine weight loss with activity modification and strength training for the best results.
Is hip replacement the only option for severe hip pain?
No - but it’s often the most reliable long-term solution when conservative methods fail and cartilage is gone. Surgery should be a last resort for younger, active people. For those over 65 with advanced arthritis (Kellgren-Lawrence Grade 4), hip replacement has excellent outcomes and can restore mobility. But if you still have some cartilage left, activity modification and physical therapy can delay or even prevent the need for surgery.
Darren McGuff
Let me tell you something most doctors won’t admit - the labrum isn’t a ‘repairable’ structure, it’s a warning light. I’ve seen 70+ patients with ‘tears’ on MRI who never had pain, and 30+ with zero tears who were screaming in the clinic. The real issue? Movement patterns. Fix the mechanics, not the tissue. That’s why activity modification works better than surgery for 80% of under-50s. Stop chasing the tear. Start chasing the motion.
Lindsey Wellmann
OMG I’m literally crying rn 😭 I’ve been doing the pillow-between-knees trick since last week and my hip hasn’t felt this good since college. Also switched to swimming - I’m now obsessed with lap counts like it’s a TikTok challenge 🏊♀️💪
Angela Stanton
Statistically, the 92% pressure increase in cadaver studies is misleading. Most cadavers are post-mortem, non-weight-bearing, and lack neuromuscular compensation. Real-world biomechanics involve proprioceptive feedback, muscle co-activation, and fascial tension - none of which are captured in ex vivo models. Also, 38% asymptomatic tears? That’s a selection bias. Most people with asymptomatic tears don’t get MRIs. The data is cherry-picked to sell PT packages.
Diana Stoyanova
Think about this: your hip isn’t a broken machine you fix with a wrench - it’s a living ecosystem. Every time you sit too low, you’re not just ‘bending your hip’ - you’re crushing the delicate synovial fluid dynamics that nourish cartilage. Every step on pavement sends shockwaves up your spine. We’ve been taught to ‘move more,’ but we’ve forgotten how to move *well*. The real revolution isn’t surgery or even PT - it’s mindfulness in motion. Learn to feel your pelvis. Notice how your glutes fire. Breathe through the movement. That’s where healing lives. Not in a clinic. Not in a scan. In your awareness.
Ashley Kronenwetter
While the article presents a compelling case for conservative management, it is imperative to acknowledge the limitations of self-reported outcomes in activity modification protocols. Without standardized biomechanical assessments, patient adherence remains highly variable. Furthermore, the absence of longitudinal data beyond five years raises questions regarding long-term joint integrity. I recommend integrating objective gait analysis and pressure mapping to validate clinical recommendations.
Heather Wilson
So let me get this straight - you’re telling me I can’t squat deep, sit cross-legged, or run? What am I supposed to do, become a yoga zombie? Also, ‘use a wedge cushion’? That’s not a solution, that’s a Band-Aid on a hernia. And why is everyone acting like this is new? I’ve been telling people this since 2018. You didn’t need a 3000-word essay to say ‘stop doing the things that hurt.’
Drew Pearlman
I was skeptical at first - I thought I’d need surgery after 5 years of hip pain. But I started doing the glute bridges every morning and switched to cycling. Three months later, I hiked 12 miles with my daughter for the first time since I was 28. I’m not cured - but I’m alive again. You don’t need to be perfect. You just need to show up. And if you’re reading this? You already are. Keep going.
Meghan Hammack
Y’all. I’m a 42-year-old mom of three. I used to hate walking because my hip felt like it was grinding glass. Now? I walk 45 minutes every morning with my dog. I use a raised toilet seat. I sit on a pillow. I do 10 clamshells before I even put my shoes on. I didn’t need a miracle. I just needed to stop punishing my body. You can do this. I believe in you.
Kiruthiga Udayakumar
Wow, this is so true. In India, we sit on the floor all the time - lotus, cross-legged, squatting. But now I see why my hip started hurting after 40. I stopped doing those poses. Now I sit on a small stool. My pain dropped 60%. Also, walking barefoot on grass helps. Natural movement > gym machines. Thank you for this.
Maggie Noe
It’s not about avoiding pain - it’s about understanding what pain is trying to tell you. The body doesn’t lie. If your hip screams when you squat, it’s not being dramatic. It’s screaming because your joint is being betrayed by decades of bad habits. We treat pain like an enemy. But what if it’s the only thing keeping you from total collapse? Listen. Adapt. Respect. That’s the real therapy.
Catherine Scutt
So you’re telling me I can’t do yoga anymore? 😒 I guess I’ll just sit here and cry into my gluten-free kale smoothie. Also, ‘swimming’? Really? That’s your solution? I’m not a dolphin. I’m a human with a life. This feels like a cult.
Elisha Muwanga
Interesting how this article ignores the role of systemic inflammation and metabolic health in joint degeneration. Obesity? Diabetes? Vitamin D deficiency? These are root causes - not just ‘bad movement.’ You can modify activity all you want, but if your insulin resistance is driving cartilage breakdown, you’re just rearranging deck chairs on the Titanic. This is reductionist medicine disguised as empowerment.





Write a comment